News
The National Institute for Health and Care Excellence (NICE) has formally recognised myCOPD within two published Early Value Assessments (EVAs) HTE18 and HTE19, providing a green light for conditional NHS commissioning of the platform during structured evidence generation. NICE has recommended myCOPD for NHS use until December 2027 while further evidence is generated.

A new partnership between leading digital health innovators, my mhealth and Patients Know Best (PKB) means shared NHS customers can streamline the delivery of their digital care tools, making it easier to empower patients to manage their health effectively. The collaboration brings together my mhealth’s award-winning self-management platforms with PKB’s personal health record solution, which is already embedded within the NHS App. “At the heart of this partnership is the patient,” said Dr. David Pettigrew, CEO of my mhealth . “By aligning our platforms, we’re enabling people to take greater control of their health while supporting clinicians with joined-up, efficient care pathways. It’s a significant step towards the NHS’s vision of a single ‘front door’ for digital health.” Key Benefits for Patients and the NHS: ● One seamless journey: Patients and clinicians benefit from a more unified experience across apps and services. ● Better outcomes through joined-up care: Shared access to data empowers more personalised and timely interventions. ● Greater access to services: Patients can engage with support tools and resources anytime, anywhere. ● Reduced clinical workload: Digitally enhanced care pathways streamline processes and free up clinical time. ● Scalable long-term condition support: Proven tools for managing COPD, asthma, diabetes, and more, integrated with national systems. ● Patient empowerment: Enabling people to be active participants in their health journey. This partnership also honours the early vision of digital health pioneer Dr Warner Slack, who said in the 1970s: “I hoped that the computer would help the doctor in the care of the patient. And in the back of my mind was the idea that the computer might actually help patients to help themselves with their medical problems.” Today , that vision is becoming reality - placing digital tools directly in the hands of patients and enabling a more connected, compassionate, and sustainable NHS. About my mhealth my mhealth provides evidence-based digital therapeutics for patients with long-term conditions including COPD, asthma, diabetes, and heart disease. Trusted by NHS organisations across the UK, their platforms deliver scalable self-management support and remote monitoring tools that improve outcomes and reduce healthcare burden. About Patients Know Best Patients Know Best is the World’s largest Personal Health Record (PHR) and patient engagement platform, integrating data feeds from over 550 health organisations and providers. The system connects information from GPs, hospitals, social and mental health care providers, to create a single, unified copy of patient data. Everything from appointments and letters to test results, care plans, real-time monitoring data and discharge summaries, as well as the patient’s own data, are all available in one patient record, enabling patients and healthcare professionals to access up-to-date health information anytime, anywhere. In the UK, the platform serves over 5 million patients, registering 100,000+ patients and releasing over 20 million test results a month. PKB integrates with the NHS App to provide a single front door for patients to access their information.

Cardiac rehabilitation is undergoing an evolution as health care systems embrace digitally enhanced programmes that promise to support patient and service outcomes. Cardiac rehabilitation (CR), a NICE recommended cornerstone in cardiovascular disease recovery and secondary prevention, has traditionally relied on in person sessions. However, there are often challenges to uptake and completion which can affect the number of people who successfully undertake and complete a programme. Digitally enhanced cardiac rehabilitation (DECR) is a modern approach that blends traditional care with digital delivery to move towards a menu-based approach to care. Leeds Community Health Care CR team were one of the early adopters of this approach, introducing the myHeart app into their pathways in 2020. ‘we started using the app as our face-to-face classes had stopped during COVID and this gave us the option for patient to access an exercise programme and cardiac information digitally. We have since restarted our face-to-face programmes, but we still offer the app as an option for our patients. It gives us wider complimentary range for our patients.’ N. Simpson - CR lead 5 years on and the team have excelled in their use of the app and have just reached the huge milestone of over 1000 patients now registered on myHeart. The way the team have utilised the app in their pathway has seen high levels of patient engagement with 84% of patients activating their account, competing over 9000 education sessions and over 12,800 activity diary entries. A recent patient survey showed the impact this is having on the patients: 92% rated the app as good or very good 85% found the apps easy to use 88% would recommend the app to others 77% said the apps have helped them to learn more about their condition 81% felt more confident in managing their condition since using the app 85% felt there has been an improvement in symptom control since using the app 81% intend to continue using the app. ‘the digital app gives our patients the choice of what they want their Cardiac Rehab to consist of and helps us make individualised programmes for our patients’ N. Simpson - CR lead Health services across the UK are working to leverage digital tools to support and enhance service delivery. Digitally enhanced cardiac rehabilitation offers services the chance to redefine recovery – offering more flexible, accessible care. For more information on this article or other my mhealth projects, please get in touch https://mymhealth.com/contact-us
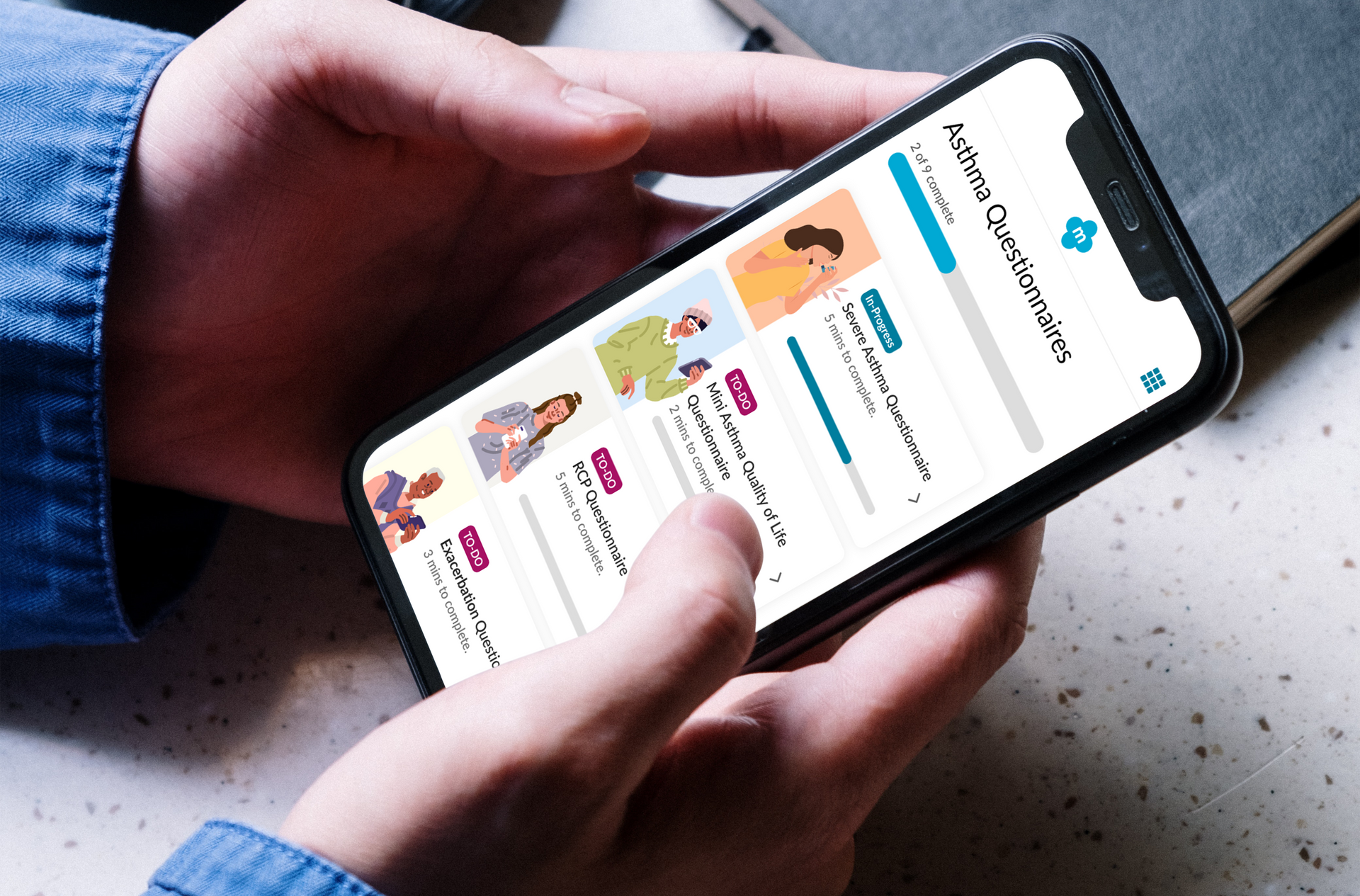
Empowering patients living with Severe Asthma: How severe asthma services are digitally transforming patient care. Living with severe asthma can be overwhelming. Frequent flare-ups, emergency health care visits and the burden of managing complex medication can take a toll – not just physically, but emotionally and mentally. Severe asthma services across the UK are working to address these challenges through the introduction of the myAsthma+ app, designed specifically to support patients with severe asthma in managing their condition more effectively and confidently. myAsthma+ combines high quality digital tools with clinical expertise to offer a range of tailored resources to support patient empowerment and improve self-management. Studies have shown that effective self-management can lead to reduced flare ups, improved quality of life and reduced unplanned health care demand (1). myAsthma+ puts evidence-based strategies into action, offering structured, easy to use tools that help patients take an active role in their care. Key features of myAsthma+ are: • Tailored education to improve health literacy • Self-management tools to track symptoms and support timely response to changes • A comprehensive series of mindfulness resources to aid stress reduction and anxiety management • Validated assessment tools to help patients and their clinicians in the management of their condition • And much more…. Over 3,300 patients have now been registered onto myAsthma+ across the UK. A recent patient survey* found that: • 84% found the app easy to use • 72% felt they had a greater understanding about their condition since using the app • 69% felt more confident in managing their condition

NHS University College London Hospitals NHS Foundation Trust, part of North Central London ICB, is taking a significant step towards enhancing patient empowerment and optimising disease management. Asthma is a chronic condition that affects millions of people worldwide, often leading to severe health complications if not managed properly. Recognising the critical need for effective self-management tools, NHS University College London Hospitals NHS Foundation Trust has chosen the myAsthma app to provide patients with the resources they need to take control of their health. Dr Kay Roy PhD FRCP, Consultant Respiratory Physician University College London Hospitals NHS Foundation Trust, comments “We are thrilled to introduce myAsthma as a self-management tool to our community. It represents a significant step forward in empowering our patients with asthma to take control of their health. By providing them with personalised support, we believe this tool will greatly improve their quality of life. Additionally, the use of myAsthma in outpatient settings will help triage patients more effectively, ensuring they are seen in a timely manner and appropriately referred for the right investigations and services. Our team is excited to see the positive impact this will have on the asthma population across North Central London ICB." The myAsthma app, part of the my mhealth suite of digital health solutions, is designed to empower patients with comprehensive tools and information to manage their asthma more effectively. Key features include: • Personalised Action Plans: Tailored asthma management plans based on individual patient needs. • Inhaler technique training: Contributing to better health outcomes and reduced risk of exacerbations • Medication Tracking: Reminders and logs to ensure patients take their medication as prescribed. • Symptom tracking: Easy-to-use tools for tracking symptoms and triggers. • Educational Resources: Access to a wealth of information on asthma, helping patients understand their condition and how to manage it. As more NHS partners embrace the my mhealth platform, we're thrilled to witness its growing impact and the positive changes it is bringing to long-term condition care. For more information on this article or other my mhealth projects, please get in touch https://mymhealth.com/contact-us
As the world changes around us, the NHS not only needs to keep up with this change but also transcend the increasing needs and demands placed on this behemoth system. I sidestepped into the world of digital technology about 6 years ago after spending a decade on the front line and experiencing firsthand the challenges of providing care with increasing demand but limited supply. To say I was naïve to the world of technology is an understatement and I very quickly came to realise that whilst the mode of delivery was different, the barriers and hurdles were not. Technology encompasses all aspects of our lives and without sounding archaic, there seems to be an app for everything! Undoubtedly this has made navigating everyday tasks easier but where does this leave healthcare and how we validate and standardise the approach to health technology?
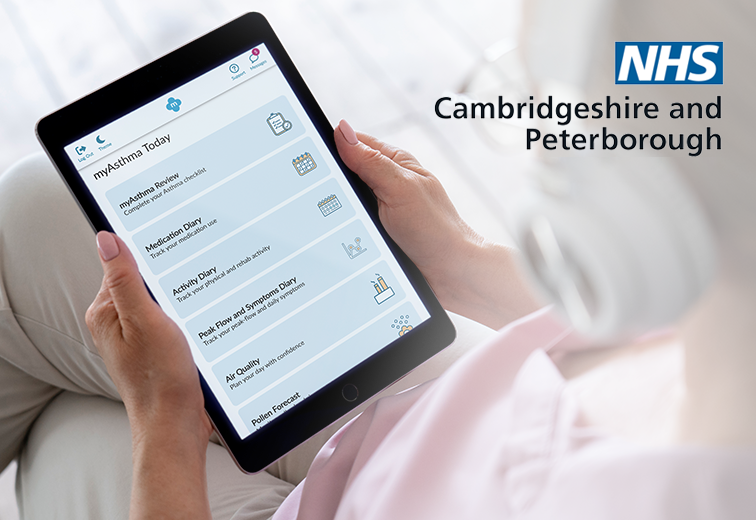
In a significant stride towards addressing health inequalities and improving asthma management, NHS Cambridgeshire & Peterborough has chosen the myAsthma app for widespread deployment across the ICS. This announcement follows the resounding success of the myAsthma Project conducted last year within the ICS. Funded by NHSx, the focus of the myAsthma Project was to target 9 primary care practices with the highest health care utilisation and level of deprivation associated with asthma in Cambridgeshire & Peterborough, to evaluate the effectiveness of the myAsthma app. Asthma is a common respiratory condition, but stark disparities in prevalence and associated healthcare outcomes are evident across the UK. Shedding light on this issue, a report from Asthma & Lung UK, titled "On the edge: how inequality affects people with asthma,"1. reveals those in deprived communities face both a higher prevalence of asthma and higher likelihood of hospitalisation. The report calls for the promotion of self-management in asthma but recognises the challenges in embedding effective self-management practices in groups with low health literacy. myAsthma, designed and developed by my mhealth, offers a self-management platform for individuals living with adult asthma, and includes expert education and inhaler technique training and much more. myAsthma has been designed to support improved health literacy, drive patient empowerment to achieve greater disease control and ultimately help reduce the frequency of exacerbations and unplanned healthcare utilisation. The results from the project were promising and have supported the case to extend the implementation across Cambridgeshire & Peterborough ICS. Dr Sripat Pai, GP Clinical Lead, Cambridgeshire & Peterborough Integrated Care System comments: "myAsthma provides our local people with asthma with the tools they need to self-manage more effectively and clinicians with a way to remotely monitor, manage and support their patients in an efficient way. The results of this pilot study have been extremely encouraging, particularly in our more deprived communities, and we look forward to seeing the impact the myAsthma App will bring once available for our wider population.” With the deployment of the myAsthma app underway across the region, Cambridgeshire & Peterborough are poised to lead the way in tackling asthma health inequalities and empower their asthma population. Supporting the implementation and rollout of the app, NHS Cambridgeshire & Peterborough have the support of the my mhealth Digital Health Advisers, who can provide workforce resource whilst driving digital literacy and inclusion. If you are interested in replicating the success of myAsthma in Cambridgeshire & Peterborough in your own service, please get in touch www.mymhealth.com/contact-us References: 1 . https://www.asthmaandlung.org.uk/sites/default/files/2023-03/auk-health-inequalities-final.pdf

This collaboration extends access to the my mhealth platform to support patients living with COPD, heart disease, and asthma, while also maintaining its support for individuals living with diabetes. The myCOPD, myAsthma, myDiabetes and myHeart apps all form part of the my mhealth digital hub, a digital therapeutic platform that provides patients with tailored, evidence-based digital interventions which improve health outcomes and reduce health service dependence. The digital hub features range from education, condition-specific intervention to rehabilitation and much more. The NHS Long Term Plan prioritises the establishment of personalised care as the norm, and promoting supported self-management is an integral part of this dedication. My mhealth’s digital hub platform is designed to make the ambitions of the Long Term Plan a reality. Through the clinical dashboards, the my mhealth platform will enable clinical teams to deliver supported self-management, track an individual patient’s response to treatment, and assess the needs of the patients and services at a population scale. These insights will, in turn, help Kent & Medway to further optimise their service delivery and prioritise care. Head of Customer Success for my mhealth, Jane Stokes comments: “We are delighted to witness the ongoing success of myDiabetes in Kent & Medway. By extending provision to patients living with asthma, COPD and cardiovascular disease, we are creating a great opportunity to help services to empower patients in their self-management, to improve their condition control and optimise their health care utilisation. We are proud to be a part of Kent’s digital transformation journey”. Ian Butcher, Senior Programme Manager & Pride Network Co-Chair Cardiovascular, Network NHS Kent & Medway adds: “All of us at Kent & Medway ICB have been delighted to witness the positive adoption of the myDiabetes self-management platform. As myDiabetes continues to prove a real success to our patients, our digital transformation journey naturally led us to collaborate as an ICB and expand these benefits to individuals dealing with Heart Disease, Asthma, and COPD. With this expansion we strive to empower an increasing number of patients throughout our region, fostering their confidence and enhancing their sense of control when it comes to their management of their long-term condition". If you want to find out more about how the my mhealth platform can support the ambitions of your health service please get in touch here, or call us on 0044 (0)1202 299 583.

myCOPD offers COPD patients the potential to manage their condition remotely, reducing the need for frequent medical visits and hospital admissions. The project aims to build capacity in both primary and secondary care settings and improve patient outcomes. The funding, provided through the SBRI Phase 3 grant, aims to explore the implementation of myCOPD, a digital therapeutic developed by my mhealth Limited, in two regions of the NHS with diverse populations and challenges. Setting 1- Acute Setting- North Bristol NHS Trust and University Hospitals Bristol and Weston NHS Foundation Trust In North Bristol NHS Trust and University Hospitals Bristol and Weston NHS Foundation Trust we will assess the value of using myCOPD in patients admitted to hospital with an exacerbation and its ability to help prevent readmissions. The primary outcome is to explore whether myCOPD supports patients to self-manage at home with clinical oversight reducing the risk of hospital readmission as part of the respiratory discharge bundle. Hospital readmission rates for patients with COPD over 12- months following discharge with change in annualised hospitalisation will be collected for those using myCOPD and those who choose not to. Data relating to each patient’s admissions during the 12 months prior to enrolment will also be collected. Secondary outcomes include benefits to the acute workforce, healthcare utilisation, welfare and quality of life scores, environmental social benefit, myCOPD app usage and usage feedback. Setting 2- Pulmonary Rehabilitation- Cornwall Partnership NHS Foundation Trust In Cornwall Partnership NHS Foundation Trust we will work with local services to provide 'digital-PR' to isolated communities and increase the capacity and access to specialist support for self-management. The primary outcome is to explore whether using a digital blended approach increases PR delivery and completion rates with improved outcome measures. The total number of patients who were offered, started and completed PR using myCOPD to support a menu-based approach will be collected. The uptake rate, completion rate and level of completion (if not 100%) will also be analysed. Secondary outcomes include admission data, healthcare resource utilisation, welfare and quality of life scores, myCOPD app usage and usage feedback. Full the full project brief please click here- https://www.weahsn.net/wp-content/uploads/2023/05/PROPEL-myCOPD_Project-Brief.pdf

We are delighted to have been shortlisted in the Health Tech World Award for “Most Improved Patient Outcomes” The award ceremony was a highly competitive event, celebrating the brightest stars in health tech and we are honoured to be among other companies that are passionate about health tech. This recognition underscores the quality, diversity, and dynamism of our sector, and we take great pride in being a part of it. We were particularly delighted to receive an honourable mention, which specifically recognized the scalability and evidence behind our platform. Scalability is a crucial aspect of any health tech solution. The my mhealth digital therapeutic platform was designed with scalability in mind, to enable implementation across various healthcare settings, reaching a wide range of patients and healthcare providers across multiple long term conditions. At my mhealth, we strive to make sure our digital therapeutics are evidence based and deliver the expected outcomes. Our dedicated research team has undertaken a number of clinical trials and real-world studies to ensure the platform is effective and able to support health services and patients. To learn more about the evidence supporting the my mhealth digital platform, please visit www.mymhealth.com/studies Being recognized for our efforts to improve patient outcomes is a testament to our commitment to delivering cutting-edge solutions that benefit patients and healthcare providers. We believe that our platform has the potential to revolutionize the healthcare industry, and we are committed to playing our part in this transformation, improving patient outcomes, and changing healthcare for the better. Thank you to the judges and congratulations to all the winners and finalists.

The my mhealth platform for long-term conditions is designed to enhance service delivery, supporting improved patient outcomes, increased patient access and engagement, resulting in improved use of healthcare resources. Founded in 2012 by two respiratory physicians, Dr Simon Bourne and Professor Tom Wilkinson set out to provide a comprehensive platform for managing respiratory conditions, to reach more patients and deliver quality care at scale. Since then, the platform has rapidly expanded to cover four major long term conditions; Asthma, COPD, diabetes and heart disease. What was the inspiration behind the my mhealth platform? Dr Simon Bourne saw the potential digital could have in his own work. “I was a respiratory consultant at the time in Southampton running the community COPD team. It became clear early that the service did not have the capacity to deliver expert care to all 6000 people diagnosed with that condition in the city. I have always been interested in tech and websites and saw this as a way of reaching a much larger population, as long as we could prove the standard of service was at least equal to a face-face intervention. So we launched my mhealth limited at Southampton Science Park, and with funding from the SBRI, built and trialled the world’s first digital therapeutic for patients with COPD”. Similarly, drawing on his own experience, Professor Tom Wilkinson comments “As a clinician caring for patients with chronic lung conditions it was clear that many patients weren’t receiving the key aspects of care they required to optimise their health. Our NHS team was expert but small and there was not enough capacity to support every patient when they needed it. The inspiration for our first app myCOPD were the patients who had become truly expert in managing their own condition, understood what to do and when to reach for help. The my mhealth platform was developed to support and empower everyone to self-manage effectively and the drive to spread that across the NHS for all patients has been the key to our progress.” What does this achievement mean? "Reaching the milestone of 100,000 registered users not only indicates a growing demand for innovative healthcare solutions but is also a testament to the company's unwavering dedication to transforming healthcare by providing cutting-edge technology and innovative solutions that address the evolving needs of patients and healthcare providers." Commenting on the journey, Professor Tom Wilkinson said: “By any standards this is a remarkable achievement which everyone in the company, our clinical partners and collaborators should be proud of. 10 years ago, Simon and I imagined that if we developed and tested digital therapeutics in the right way we could support more patients than we ever could using conventional models of care. That vision is now a reality. A clinician can see 10-20 patients in a clinic- and may get to review a patient every six months or more. With the my mhealth platform we can help support 100,000 users daily and that number is growing exponentially now. That’s a lifetime of a practitioner’s positive clinical impact delivered everyday of the year- which is such a great outcome.” Dr Simon Bourne shares his thoughts: “This is a huge milestone in the history of digital therapeutics. We knew that the digital therapeutics, once in the hands of patients could improve the outcomes and symptoms of patients, and once a patient was invited to download the app, activation and engagement was excellent. The problem to solve was, how do we get this to patients with a confirmed diagnosis of the condition. It took us a while to develop the solutions with NHS partners that would enable us to scale to more than 100,000 users. The key was the development of a new role, known as a digital health adviser, who work between the digital therapeutic, the patient and the service to drive uptake and engagement”. What’s next for my mhealth? The company is well positioned to continue leading the way in digital therapeutics and making a positive impact on the lives of many worldwide. “We are deploying our digital therapeutics for long-term conditions now across more ICB footprints this year. Working with NHS partners we can now scale this to improve outcomes of patients, and within current budget constraints. We are planning our US launch, initially with myCOPD and translating our myHeart app with European clinical teams to enter clinical trials soon. With NIHR funding, through the NHSx AI awards we are also investigating other solutions to improve the outcomes of patients with COPD”. Said Dr Simon Bourne. Looking to the future, Professor Tom Wilkinson comments “The real impacts of our work are ahead- we are rapidly growing our user base, working with more and more clinical teams and synergistically driving an evolution into digitally enhanced care at a time the NHS really needs it. Excitingly are expanding overseas to India, the US and into Europe, building our evidence base for efficacy and value as we go. For a decade we have been at the vanguard of digital therapeutic development and delivery and in another 10 years we aim to be a major contributor to improvements in global health”.

SBRI Healthcare , an Accelerated Access Collaborative initiative, in partnership with the Academic Health Science Networks (AHSNs) and Asthma + Lung UK , has selected my mhealth Limited as one of their grant recipients to support respiratory patients. The SBRI Healthcare ‘Competition 21, Phase 3 for Real-world Testing and Implementation: Respiratory Diseases’ identifies the most promising innovations that will help the NHS continue to evolve, meet more patient needs whilst addressing some of the biggest healthcare challenges; one of which is respiratory diseases. With up to half of all hospital beds being occupied by patients with respiratory illnesses, supporting discharges, preventing disease exacerbations and readmissions is key to ensuring the NHS can manage the huge number of patients needing help. myCOPD, a digital therapeutic from my mhealth, can support this. The funding from SBRI Healthcare will be used to support real-world testing and implementation of my mhealth's platform in respiratory care pathways across the UK. The goal of the project is to measure the clinical and economic benefits of digital therapeutics in respiratory care, which will help to pave the way for widespread adoption across the NHS. "We are thrilled to have been awarded this funding by SBRI Healthcare, which will allow us to accelerate the adoption of our digital therapeutic platform in the UK. We believe that our platform has the potential to revolutionize respiratory care management" said Professor Tom Wilkinson, Professor & Honorary NHS Consultant Respiratory Medicine Southampton University Faculty of Medicine and my mhealth's Chief Science Officer and Co-Founder. "myCOPD is a powerful tool and we are excited to work with healthcare providers in Bristol and Cornwall to demonstrate its impact on patient outcomes and reduce the burden on the NHS. We would like to thank the West of England AHSN for their support throughout the funding process and look forward to working with the NHS and other healthcare partners to bring our digital therapeutic platform to more patients across the UK. The implementation of myCOPD into respiratory care pathways will be explored in two distinct UK regions, Bristol & Cornwall." Cheryl Scott, Industry and Innovation Lead at the West of England AHSN added: "We’re delighted that my mhealth has been successful in securing this funding in order to support people with respiratory diseases and our health and care delivery partners in the West of England. We continue to p rovide support and look forward to seeing the impacts of the research study.” my mhealth is also working with NICE to develop the evidence and health economic model required to support the national roll out of my COPD. If you want to find out more about this project or learn how myCOPD can help your respiratory patients, please get in touch here.

Simon Bourne, Company President at my mhealth comments: “As a respiratory focussed digital therapeutics company, we are honoured to have been chosen to roll out our product nationally to better support patients on biologics, who are living with Severe Asthma. We have already seen the huge potential of digital therapeutics to improve patients’ symptoms and quality of life and deliver efficiencies across primary and community health care services, and look forward to working with the specialist severe asthma centres across the UK." Professor James Dodd, clinical lead North Bristol’s complex airways service added: “The Bristol severe Asthma service is delighted to be part of this national project to adopt and evaluate the myAsthma Biologic App. With the growing number of highly effective monoclonal antibody therapies, and the growing demand on our services, we believe that digital therapeutics like myAsthma Biologic will be increasingly important. Digital innovation has the potential to complement our dedicated multi-disciplinary team to increase capacity and enhance the support patients need to keep them well.” About my mhealth my mhealth’s digital therapeutics have been prescribed to over 90,000 patients with chronic conditions, resulting in reduced morbidity and hospital admissions. It serves patients across a range of long-term conditions, including COPD, asthma, diabetes and cardiovascular disease. Real world and clinical trial evidence demonstrates the efficacy of digital interventions on the my mhealth platform. For more information on my mhealth, visit www.mymhealth.com

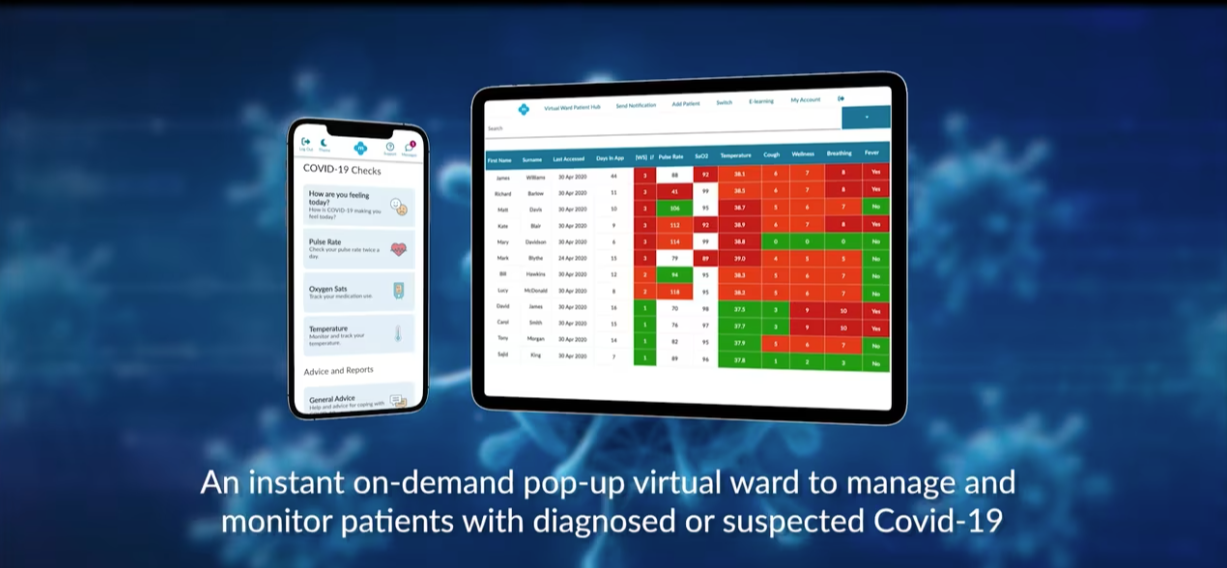
my mhealth , a leading Digital Therapeutics (DTx) company based in the UK, is pleased to announce the promotion of Dr. David Pettigrew as CEO. David will guide the organisation in its mission to improve the quality of care for people with long term conditions, through digital health. Having spent time in the US successfully growing a healthcare technology business for a UK-based company, David is ideally placed to lead my mhealth’s expansion into the US market. Dr. Pettigrew has a broad and extensive experience in the digital health industry. Throughout his 17 year career, he has been responsible for managing large and complex digital health product development projects, building new organisational capabilities and for overall business delivery. He was an early pioneer in developing FDA-regulated smartphone apps. Most recently, he led Sagentia, an AIM-listed international technology and product development business, and was part of BrightInsight’s leadership team, focusing on building DTx solutions for the medtech and pharmaceutical industry. David holds a DPhil in Molecular Biophysics from the University of Oxford. David replaces the founder Simon Bourne, who is transitioning to President and will continue to take an active interest in developing my mhealth’s next generation AI capabilities. Bourne commented: "When I co-founded my mhealth over 10 years ago we set out to transform healthcare using digital platforms. Back then this was through a simple website developed to support COPD patients. We never imagined back then how much this simple tool would transform the lives of patients. Following successful randomised clinical trials and NHS National Innovation Accelerator adoption, my mhealth has supported over 80,000 patients and multiple long-term conditions across the UK. During the pandemic, we delivered access to digital rehabilitation, when most services had to close. We are also proud of the contribution we made in easing capacity pressures in the NHS through our COVID virtual ward remote monitoring solution. Today marks an important event in our history, as I hand over the CEO role to David Pettigrew. David has a proven track record, and having worked with him over the last 5 months in his role as Chief Strategy Officer, I have every confidence he will take my mhealth to the next level." Pettigrew stated: " Having spent 17 years developing DTx solutions, I can confidently say that no other company has been as successful as my mhealth in building such a vast and engaged user base. I would like to take this opportunity to thank Simon and the team for all their hard work to bring the company to where it is today. I’m honoured to be taking on the responsibility of leading my mhealth in the next stage of its journey, which will focus on launching in the US and beyond, expanding our relationship with the NHS and extending our data and clinical trial partnerships with the pharmaceutical industry. Our primary mission will continue to be improving the lives of patients with long term conditions everywhere." About my mhealth my mhealth’s digital therapeutics have been prescribed to over 80,000 patients with chronic conditions, resulting in reduced morbidity and hospital admissions. It serves patients across a range of long term conditions, including COPD, asthma, diabetes and cardiovascular disease. Our flagship product, myCOPD, was the exclusive digital therapeutic deployed by the UK’s NHS to deliver pulmonary rehabilitation during the pandemic, when in person care was practically inaccessible. Real world and clinical trial evidence demonstrates the efficacy of digital interventions on the my mhealth platform. For more information on my mhealth, visit www.mymhealth.com

Results demonstrated that self-reported COPD data, using a digital health app, can be used to identify users at risk of exacerbation within 3 days with moderate discriminative ability (AUROC 0.727, 95% CI 0.720-0.735). Further research utilising additional linked data (particularly from medical devices such as smart inhalers, physiological monitoring sensors, and environmental sensors) are expected to increase the accuracy of these models. Data self-reported to health care apps designed to remotely monitor patients with COPD can be used to predict acute exacerbation events with moderate performance. This could increase personalisation of care by allowing pre-emptive action to be taken to mitigate the risk of future exacerbation events. With the Health and Social Care Secretary setting a target for 4 million to benefit from personalised care by March 2024, leveraging the data collected by these apps in prognostic models could provide increased personalisation of care by allowing pre-emptive action to be taken to mitigate the risk of future exacerbation events

Evaluation of myCOPD - a positive population health management approach to the remote monitoring of patients with COPD. The study showed a positive uptake and usage with myCOPD, demonstrating improvement in CAT scores. Socioeconomic factors did not appear to negatively influence app activation. See results from Dorset Intelligence and Insight Service (DiiS) and my mhealth collaboration, supporting the remote monitoring of patients with COPD. About my mhealth my mhealth’s digital therapeutics have been prescribed to over 90,000 patients with chronic conditions, resulting in reduced morbidity and hospital admissions. It serves patients across a range of long-term conditions, including COPD, asthma, diabetes and cardiovascular disease. Real world and clinical trial evidence demonstrates the efficacy of digital interventions on the my mhealth platform. For more information on my mhealth, visit www.mymhealth.com

A new partnership between Vitality and Bournemouth-based digital healthcare pioneer my mhealth offers Vitality members access to an entire suite of cutting-edge digital therapeutics designed to manage long-term health conditions. Vitality members will receive a 50% discount on annual subscriptions to any of the my mhealth apps: myCOPD, myDiabetes, myHeart, myAsthma and, myOp. Each app provides members with a unique and tailored evidence-based digital intervention that's proven to improve health outcomes using a broad range of self-management tools including medicine optimisation, rehabilitation, education, risk-factor modification, condition-specific interventions, care planning and more. Commenting on the partnership, Vitality's Head of Healthcare Strategy, Bianca Grotepass said: "There has been an increase in the number of digital therapeutics that people can use to take control of their long-term health conditions, and it’s clear that by working with my mhealth we can now offer our members access to the tools that enable them to do just that." "By using clinically proven digital therapeutics such as myCOPD and myHeart, Vitality members can improve their quality of life by tracking their symptoms, understanding their condition and learning how to better manage their health." Simon Bourne, CEO of my mhealth added: "Vitality’s ambition to be a force for social good and empower their members to develop long-term healthy habits resonates with our own ambitions to change healthcare forever. We’re proud to be able to offer Vitality members another platform that will help them make a real difference to their quality of life." If you want to find out how my mhealth can help you, please get in touch here or call us on +44 (0)1202 299 583.

NHSX Digital Health Partnership Award funds the adoption of both myOp and myCOPD in four NHS centres
The NHSX Innovation Development Team has launched the Digital Health Partnership Award. This has been created to help NHS organisations in England to bid for funding to accelerate the adoption of digital health technologies to support patients with long term conditions focusing on supporting people at home. The Award brings together partners critical to the scaling of digital health technology. my mhealth have partnered with North Bristol NHS Trust, University Hospital Southampton NHS Foundation Trust (UHS), Norfolk and Norwich University Hospital NHS Foundation Trust and University Hospital of North Midlands NHS Trust to secure funding from NHSX that will enable the adoption of myOp, an app that supports the prehabilitation of patients prior to elective surgery, and myCOPD, a digital therapeutic for patients with Chronic Obstructive Pulmonary Disease (COPD). COPD Self-management myCOPD helps people living with COPD to perfect their inhaler technique with easy-to-follow inhaler videos and helps them to manage their COPD using a variety of interventions such as online pulmonary rehabilitation classes. To promote digital healthcare North Bristol NHS Trust are introducing myCOPD to patients with COPD. This will support patients who have been admitted to hospital with their COPD, enhancing their recovery at home and reducing their risk of readmission. Patient activation and adoption will be analysed by University of Bath, and the West of England AHSN will report on the outcomes, benefits, and evidence of impact realisation. Surgical Prehabilitation myOp is a universal intervention which gives people waiting for elective surgery the tools they need to prepare and recover faster. myOp includes a series of screening tools which clinicians can use to rapidly risk stratify and identify patients at a higher risk of complications. These patients can then be supported with targeted support and interventions. UHS will deliver this intervention to patients undergoing certain types of surgery. The aim is to initially support patients to use technology to prepare for surgery and improve their physical and mental health. Results will be analysed by UHS alongside Norfolk and Norwich University Hospital NHS Foundation Trust and University Hospital of North Midlands NHS Trust my mhealth CEO Simon Bourne commented, "We’ve witnessed digital services like myCOPD and myOp achieve great adoption across the UK and thanks to the funding provided by the Digital Health Partnership Award digital therapeutics will be available to even more people living with long-term conditions or waiting for surgery." Dr Harry Thirkettle, the mind behind of myOp added, "Up to 30% of surgical patients experience some form of complication after surgery, leading to increased healthcare costs and a longer stay in hospital for the patient. With Covid-19 leading to huge waiting lists and a backlog of elective surgery, it's more important than ever that we find ways to improve efficiency, reduce complications and length of stay. A variety of prehabilitation interventions can reduce complication rates by up to 50%. We’ve combined these interventions into a single app and we’re confident that with this award, we’ll be able to support many more people from decision to operate to full recovery." If you want to find out more about this award or how myOp and myCOPD can help your patients or if you need support with an NHSX award application to support your health service's digital transformation, please get in touch here or call us on +44 (0)1202 299 583.

In 2018, Southend University Hospital introduced myCOPD , a new menu-based pulmonary rehabilitation delivery model to provide options for patients who were unable to attend the traditional centre-based classes. myCOPD was designed to address the challenges faced with service capacity and completion rates. The Southend DEPR (Digitally Enhanced Pulmonary Rehabilitation) model is an exemplar of innovation which has demonstrated an ability to rise to increasing service demand, maintain service delivery quality and provide resilience in the face of unforeseen events, such as COVID-19.