my mhealth release new instant, on-demand pop-up virtual ward service to manage and monitor patients with diagnosed or suspected COVID-19
5 Aug, 2020
Available to license directly from my mhealth or from the CCS Spark DPS, COVID-19 Virtual Ward is already helping people across the UK
With the possibility that further waves of COVID-19 will cause yet more disruption to the health service, my mhealth have enhanced their COVID-19 virtual ward app. This new product combines an upgraded app with a wraparound support package, that enables clinical teams to open a virtual ward within 48 hours to safely manage and monitor patients with COVID-19 at home, or in a care home.
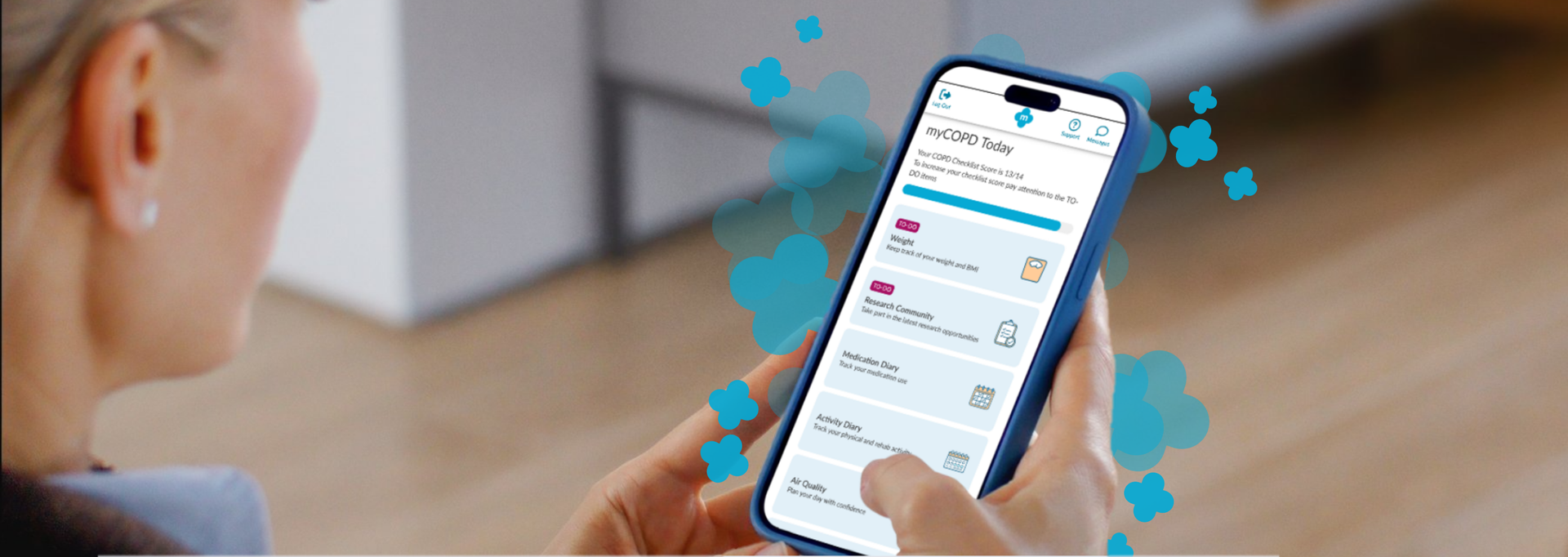
The patient is given access to an app that can be used on almost any device (smartphone, tablet, or computer) which records their symptoms as well as observations from a pulse oximeter, twice a day. The app instantly provides patients and their care team with messages/alerts aligned to the new NHS England COVID-19 Remote Monitoring Guidelines
The COVID-19 Virtual Ward comes with a full customer support program for both the clinical site and the patient. Not only have we further refined the application to meet the needs of clinical teams and patients, but we have also streamlined our deployment processes meaning a COVID-19 Virtual Ward can be set up and ready to receive patients within 48 hours, guaranteed. Each patient is supplied with a pulse oximeter directly from us within 24 hours, and we facilitate the admission by assisting patients in using the app and the pulse-oximeter. Patients can be discharged from the ward at any time, and a copy of their stay can now be exported to the clinical record.
On contract signature we will work with clinical teams, local information and clinical governance leads to get all of the approvals, training and permissions in place, so when NHS providers need to activate the ward, all of these processes are covered, reducing the risk of any unnecessary delays.
"This new product is a game-changer for the safe remote management of patients with COVID-19, and combined with our integrated long-term condition platform can optimise patients most at risk during their virtual stay"
COVID-19 Virtual Wards are set up for a one-off fixed fee and can be activated at any time over a 3-year period. The cost includes site setup, training, and the postage/distribution of a pulse oximeter for each patient.
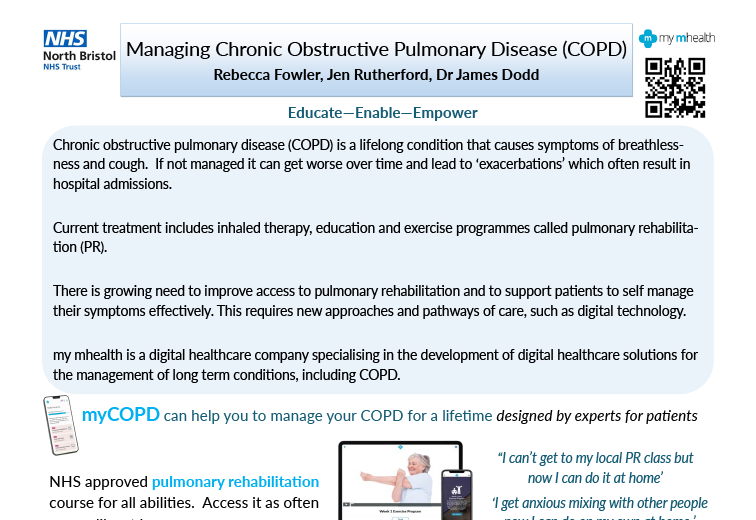
The National Institute for Health and Care Excellence (NICE) has formally recognised myCOPD within two published Early Value Assessments (EVAs) HTE18 and HTE19, providing a green light for conditional NHS commissioning of the platform during structured evidence generation. NICE has recommended myCOPD for NHS use until December 2027 while further evidence is generated.

A new partnership between leading digital health innovators, my mhealth and Patients Know Best (PKB) means shared NHS customers can streamline the delivery of their digital care tools, making it easier to empower patients to manage their health effectively. The collaboration brings together my mhealth’s award-winning self-management platforms with PKB’s personal health record solution, which is already embedded within the NHS App. “At the heart of this partnership is the patient,” said Dr. David Pettigrew, CEO of my mhealth . “By aligning our platforms, we’re enabling people to take greater control of their health while supporting clinicians with joined-up, efficient care pathways. It’s a significant step towards the NHS’s vision of a single ‘front door’ for digital health.” Key Benefits for Patients and the NHS: ● One seamless journey: Patients and clinicians benefit from a more unified experience across apps and services. ● Better outcomes through joined-up care: Shared access to data empowers more personalised and timely interventions. ● Greater access to services: Patients can engage with support tools and resources anytime, anywhere. ● Reduced clinical workload: Digitally enhanced care pathways streamline processes and free up clinical time. ● Scalable long-term condition support: Proven tools for managing COPD, asthma, diabetes, and more, integrated with national systems. ● Patient empowerment: Enabling people to be active participants in their health journey. This partnership also honours the early vision of digital health pioneer Dr Warner Slack, who said in the 1970s: “I hoped that the computer would help the doctor in the care of the patient. And in the back of my mind was the idea that the computer might actually help patients to help themselves with their medical problems.” Today , that vision is becoming reality - placing digital tools directly in the hands of patients and enabling a more connected, compassionate, and sustainable NHS. About my mhealth my mhealth provides evidence-based digital therapeutics for patients with long-term conditions including COPD, asthma, diabetes, and heart disease. Trusted by NHS organisations across the UK, their platforms deliver scalable self-management support and remote monitoring tools that improve outcomes and reduce healthcare burden. About Patients Know Best Patients Know Best is the World’s largest Personal Health Record (PHR) and patient engagement platform, integrating data feeds from over 550 health organisations and providers. The system connects information from GPs, hospitals, social and mental health care providers, to create a single, unified copy of patient data. Everything from appointments and letters to test results, care plans, real-time monitoring data and discharge summaries, as well as the patient’s own data, are all available in one patient record, enabling patients and healthcare professionals to access up-to-date health information anytime, anywhere. In the UK, the platform serves over 5 million patients, registering 100,000+ patients and releasing over 20 million test results a month. PKB integrates with the NHS App to provide a single front door for patients to access their information.

Cardiac rehabilitation is undergoing an evolution as health care systems embrace digitally enhanced programmes that promise to support patient and service outcomes. Cardiac rehabilitation (CR), a NICE recommended cornerstone in cardiovascular disease recovery and secondary prevention, has traditionally relied on in person sessions. However, there are often challenges to uptake and completion which can affect the number of people who successfully undertake and complete a programme. Digitally enhanced cardiac rehabilitation (DECR) is a modern approach that blends traditional care with digital delivery to move towards a menu-based approach to care. Leeds Community Health Care CR team were one of the early adopters of this approach, introducing the myHeart app into their pathways in 2020. ‘we started using the app as our face-to-face classes had stopped during COVID and this gave us the option for patient to access an exercise programme and cardiac information digitally. We have since restarted our face-to-face programmes, but we still offer the app as an option for our patients. It gives us wider complimentary range for our patients.’ N. Simpson - CR lead 5 years on and the team have excelled in their use of the app and have just reached the huge milestone of over 1000 patients now registered on myHeart. The way the team have utilised the app in their pathway has seen high levels of patient engagement with 84% of patients activating their account, competing over 9000 education sessions and over 12,800 activity diary entries. A recent patient survey showed the impact this is having on the patients: 92% rated the app as good or very good 85% found the apps easy to use 88% would recommend the app to others 77% said the apps have helped them to learn more about their condition 81% felt more confident in managing their condition since using the app 85% felt there has been an improvement in symptom control since using the app 81% intend to continue using the app. ‘the digital app gives our patients the choice of what they want their Cardiac Rehab to consist of and helps us make individualised programmes for our patients’ N. Simpson - CR lead Health services across the UK are working to leverage digital tools to support and enhance service delivery. Digitally enhanced cardiac rehabilitation offers services the chance to redefine recovery – offering more flexible, accessible care. For more information on this article or other my mhealth projects, please get in touch https://mymhealth.com/contact-us
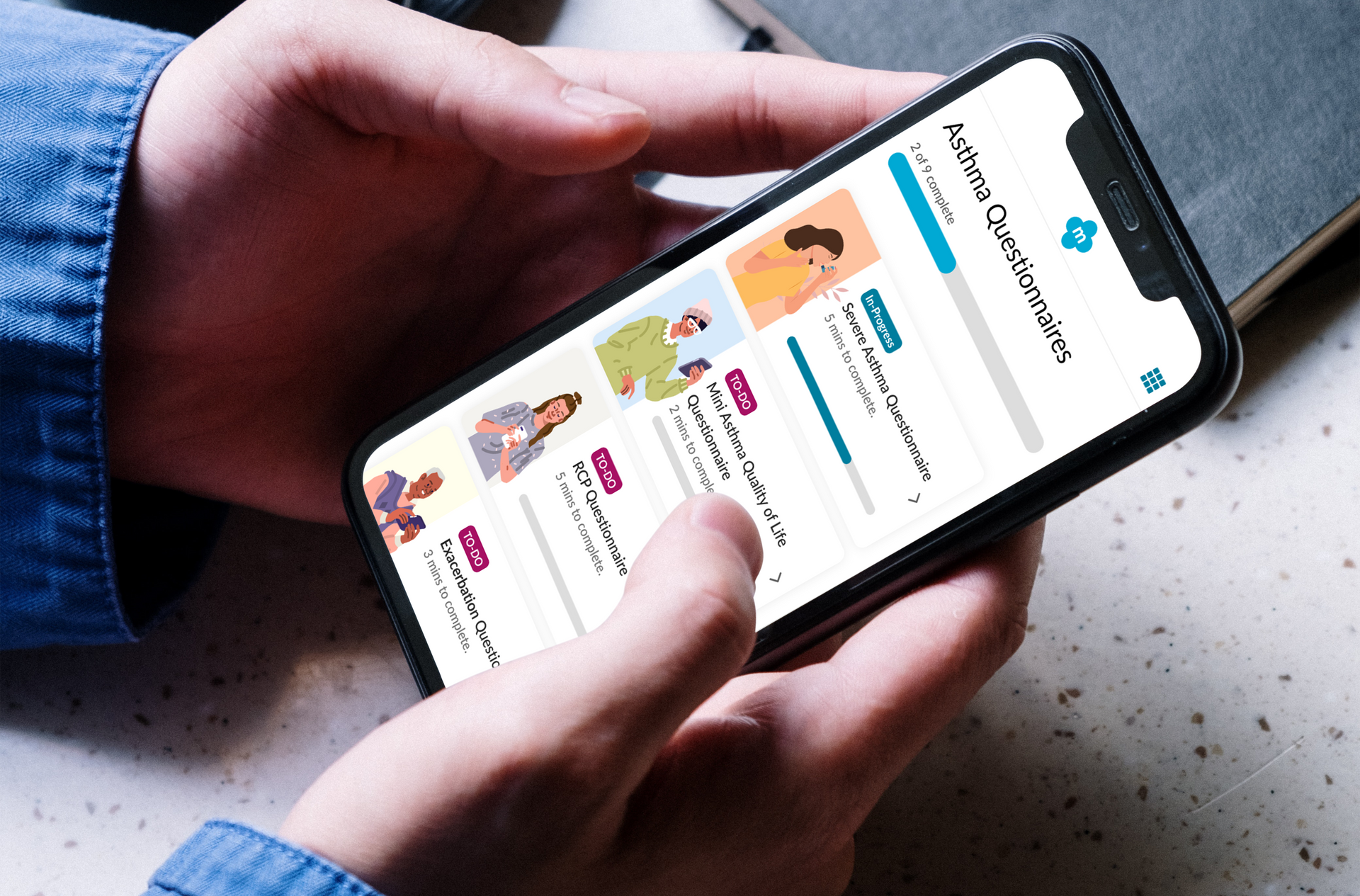
Empowering patients living with Severe Asthma: How severe asthma services are digitally transforming patient care. Living with severe asthma can be overwhelming. Frequent flare-ups, emergency health care visits and the burden of managing complex medication can take a toll – not just physically, but emotionally and mentally. Severe asthma services across the UK are working to address these challenges through the introduction of the myAsthma+ app, designed specifically to support patients with severe asthma in managing their condition more effectively and confidently. myAsthma+ combines high quality digital tools with clinical expertise to offer a range of tailored resources to support patient empowerment and improve self-management. Studies have shown that effective self-management can lead to reduced flare ups, improved quality of life and reduced unplanned health care demand (1). myAsthma+ puts evidence-based strategies into action, offering structured, easy to use tools that help patients take an active role in their care. Key features of myAsthma+ are: • Tailored education to improve health literacy • Self-management tools to track symptoms and support timely response to changes • A comprehensive series of mindfulness resources to aid stress reduction and anxiety management • Validated assessment tools to help patients and their clinicians in the management of their condition • And much more…. Over 3,300 patients have now been registered onto myAsthma+ across the UK. A recent patient survey* found that: • 84% found the app easy to use • 72% felt they had a greater understanding about their condition since using the app • 69% felt more confident in managing their condition

Results of a service evaluation using myHeart in a large London-based acute NHS Trust. We are pleased to report the outcomes from this recent service evaluation of myHeart and the potential benefit of using the myHeart app to supplement existing cardiac rehabilitation (CR). Cardiac rehabilitation is an essential evidence-based intervention that supports patient recovery following a cardiac event. It offers patients a structured education and exercise programme to aid recovery and support behavioural changes to help reduce the risk of future cardiac health complications. The myHeart app provides a structure educational and exercise intervention that mirrors current CR service delivery as well as supportive self-management tools. Overall, 721 patients were invited to participate in 1 of 4 groups (class-based CR, class-based CR with myHeart, home-based CR and home-based CR with myHeart). A total of 584 patients opted to use class-based CR and of these 43 chose to include myHeart to support them with this. There were 137 patients in the home-based group, with 54 choosing to include myHeart alongside their CR. This 12-week evaluation involved functional, physical and psychological assessments both before and after CR to explore potential changes. Patients were also asked to complete a rating of perceived exertion Borg RPE scale (Borg 6-20). Those in the home-based groups were contacted mid-way through the study. Results identified three key outcomes: 1. Blood pressure, cholesterol, LDL, BMI, HbA1c and exercise were all very similar across the groups with marginal differences across each measure. 2. Drop-out rates (DOR) of patients being invited to attend CR and attending CR were significantly lower in those groups with access to myHeart. * Class only: DOR = 58.2% Class + App; DOR = 25.6% * Home only: DOR = 73.5% Home + App; DOR = 42.6% 3. Those patients with access to myHeart and in the home-based group saw the greatest improvement in anxiety and depression scores. This real-world evaluation provides an encouraging insight into the potential impact of myHeart to supplement CR services, and is suggestive that, as an adjunct to support both class and home-based programmes, myHeart helps to reduce drop-out rates in CR and can assist in reinforcing continuous engagement with CR programmes.