my mhealth launches COPD app in New Zealand in partnership with Vodafone and district health board
9 Sep, 2021
myCOPD is the first digital self-management programme for COPD to be available in New Zealand
Digital therapeutics pioneer my mhealth has announced the first international rollout of its digital therapeutic,
myCOPD in New Zealand. The rollout is initially focused on the Māori and Pasifika population, a first for a British made digital self-management programme designed specifically for COPD.
Within one District Health Board (DHB), around 300
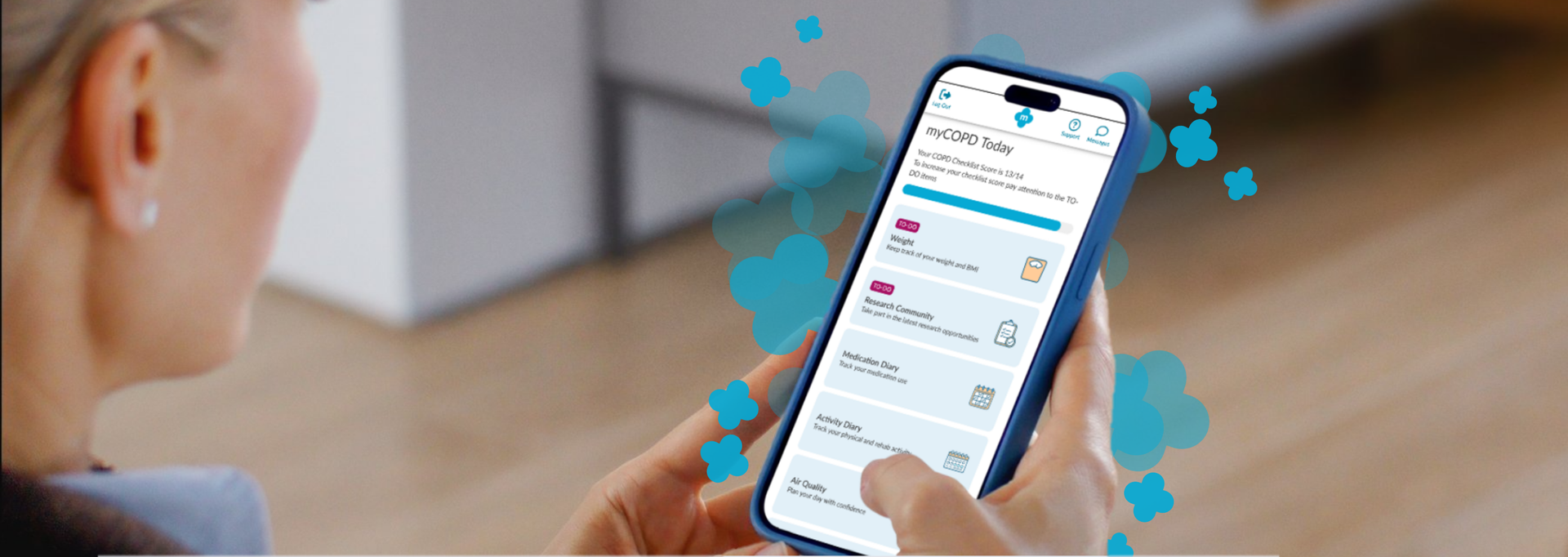
patients will be the first in the country to have access to the app, with an aim to expand patient access. Over the last 2 years of working closely together, with COVID impacting initial launch plans, my mhealth and the leading DHB have the first COPD patients now benefiting from the online therapeutic. myCOPD provides patients with access to a digital self-management programme, perfecting inhaler technique with easy-to-follow inhaler videos, access to online pulmonary rehabilitation and learning how to manage their COPD from world experts. All of this enables healthcare professionals to remotely monitor symptoms of COPD, evolve and enhance service access for patients.
COPD is a major respiratory disease in New Zealand. An estimated 15% (200,000) of all New Zealanders aged over 45 years suffer from the condition and is the fourth leading cause of death in the region behind cancer, heart disease and stroke. The DHB set out to find a new digital solution to improve patient care as well as reducing costs of unnecessary admissions and discrepancies surrounding the access to and availability of healthcare. Following investment from Vodafone New Zealand, the clear objective is to improve the health of COPD patients and their access to services, with part of the population disproportionately affected with a prevalence twice that of other ethnic groups1.
The DHB selected myCOPD as the chosen solution, as the platform provides the key requirements local patients asked for, as well as the capacity to serve as a blueprint for other chronic conditions such as heart failure and diabetes. All of these have similar needs that are currently not being met due to lack of sufficient funding. Currently in the UK the app is used by over 50,000
people, improving the quality of care and the frequency of their check-ins.
Global Lead for my mhealth, Ian Thompson, commented:
"All of us here at my mhealth are excited to bring myCOPD into New Zealand and into the respiratory teams hands at the DHB. We have been working together for almost 2 years to get this moving; the global pandemic prevented us getting started a year ago, but through hard work by all involved, we have finally got the first patients on board myCOPD.
The main part of our work is focused on ensuring adaptations that are needed to the platform meet the needs of the Māori and Pasifika populations. We also want to recognise the support from Vodafone NZ, who have provided funds for this initial program. This support from Vodafone NZ puts the local digital health economy on its first steps towards its digital evolution, supporting the access of services into the homes of patients across the DHB and beyond for those suffering with COPD. This is something we have been doing with the NHS for a number of years and hope our learnings can accelerate the digital adoption."
Chief Enterprise Officer at Vodafone NZ, Lindsay Zwart, added:
"We’re constantly looking out for world-class digital solutions to enhance the lives of New Zealanders, and my mhealth exemplifies this approach. This initial deployment with the DHB will enable us to test whether the myCOPD app can help to improve the health and future outcomes for COPD patients in the region, and if this technology can be rolled out further around New Zealand."
If you're a healthcare professional or clinician and want to know more about how myCOPD can help your patients - anywhere in the world, you can find out more at www.mymhealth.com or by calling my mhealth on 0044 (0)1202 299 583
References
1. Nation Health Committee (2013) Respiratory Disease in New Zealand
The National Institute for Health and Care Excellence (NICE) has formally recognised myCOPD within two published Early Value Assessments (EVAs) HTE18 and HTE19, providing a green light for conditional NHS commissioning of the platform during structured evidence generation. NICE has recommended myCOPD for NHS use until December 2027 while further evidence is generated.

A new partnership between leading digital health innovators, my mhealth and Patients Know Best (PKB) means shared NHS customers can streamline the delivery of their digital care tools, making it easier to empower patients to manage their health effectively. The collaboration brings together my mhealth’s award-winning self-management platforms with PKB’s personal health record solution, which is already embedded within the NHS App. “At the heart of this partnership is the patient,” said Dr. David Pettigrew, CEO of my mhealth . “By aligning our platforms, we’re enabling people to take greater control of their health while supporting clinicians with joined-up, efficient care pathways. It’s a significant step towards the NHS’s vision of a single ‘front door’ for digital health.” Key Benefits for Patients and the NHS: ● One seamless journey: Patients and clinicians benefit from a more unified experience across apps and services. ● Better outcomes through joined-up care: Shared access to data empowers more personalised and timely interventions. ● Greater access to services: Patients can engage with support tools and resources anytime, anywhere. ● Reduced clinical workload: Digitally enhanced care pathways streamline processes and free up clinical time. ● Scalable long-term condition support: Proven tools for managing COPD, asthma, diabetes, and more, integrated with national systems. ● Patient empowerment: Enabling people to be active participants in their health journey. This partnership also honours the early vision of digital health pioneer Dr Warner Slack, who said in the 1970s: “I hoped that the computer would help the doctor in the care of the patient. And in the back of my mind was the idea that the computer might actually help patients to help themselves with their medical problems.” Today , that vision is becoming reality - placing digital tools directly in the hands of patients and enabling a more connected, compassionate, and sustainable NHS. About my mhealth my mhealth provides evidence-based digital therapeutics for patients with long-term conditions including COPD, asthma, diabetes, and heart disease. Trusted by NHS organisations across the UK, their platforms deliver scalable self-management support and remote monitoring tools that improve outcomes and reduce healthcare burden. About Patients Know Best Patients Know Best is the World’s largest Personal Health Record (PHR) and patient engagement platform, integrating data feeds from over 550 health organisations and providers. The system connects information from GPs, hospitals, social and mental health care providers, to create a single, unified copy of patient data. Everything from appointments and letters to test results, care plans, real-time monitoring data and discharge summaries, as well as the patient’s own data, are all available in one patient record, enabling patients and healthcare professionals to access up-to-date health information anytime, anywhere. In the UK, the platform serves over 5 million patients, registering 100,000+ patients and releasing over 20 million test results a month. PKB integrates with the NHS App to provide a single front door for patients to access their information.

Cardiac rehabilitation is undergoing an evolution as health care systems embrace digitally enhanced programmes that promise to support patient and service outcomes. Cardiac rehabilitation (CR), a NICE recommended cornerstone in cardiovascular disease recovery and secondary prevention, has traditionally relied on in person sessions. However, there are often challenges to uptake and completion which can affect the number of people who successfully undertake and complete a programme. Digitally enhanced cardiac rehabilitation (DECR) is a modern approach that blends traditional care with digital delivery to move towards a menu-based approach to care. Leeds Community Health Care CR team were one of the early adopters of this approach, introducing the myHeart app into their pathways in 2020. ‘we started using the app as our face-to-face classes had stopped during COVID and this gave us the option for patient to access an exercise programme and cardiac information digitally. We have since restarted our face-to-face programmes, but we still offer the app as an option for our patients. It gives us wider complimentary range for our patients.’ N. Simpson - CR lead 5 years on and the team have excelled in their use of the app and have just reached the huge milestone of over 1000 patients now registered on myHeart. The way the team have utilised the app in their pathway has seen high levels of patient engagement with 84% of patients activating their account, competing over 9000 education sessions and over 12,800 activity diary entries. A recent patient survey showed the impact this is having on the patients: 92% rated the app as good or very good 85% found the apps easy to use 88% would recommend the app to others 77% said the apps have helped them to learn more about their condition 81% felt more confident in managing their condition since using the app 85% felt there has been an improvement in symptom control since using the app 81% intend to continue using the app. ‘the digital app gives our patients the choice of what they want their Cardiac Rehab to consist of and helps us make individualised programmes for our patients’ N. Simpson - CR lead Health services across the UK are working to leverage digital tools to support and enhance service delivery. Digitally enhanced cardiac rehabilitation offers services the chance to redefine recovery – offering more flexible, accessible care. For more information on this article or other my mhealth projects, please get in touch https://mymhealth.com/contact-us
Empowering patients living with Severe Asthma: How severe asthma services are digitally transforming patient care. Living with severe asthma can be overwhelming. Frequent flare-ups, emergency health care visits and the burden of managing complex medication can take a toll – not just physically, but emotionally and mentally. Severe asthma services across the UK are working to address these challenges through the introduction of the myAsthma+ app, designed specifically to support patients with severe asthma in managing their condition more effectively and confidently. myAsthma+ combines high quality digital tools with clinical expertise to offer a range of tailored resources to support patient empowerment and improve self-management. Studies have shown that effective self-management can lead to reduced flare ups, improved quality of life and reduced unplanned health care demand (1). myAsthma+ puts evidence-based strategies into action, offering structured, easy to use tools that help patients take an active role in their care. Key features of myAsthma+ are: • Tailored education to improve health literacy • Self-management tools to track symptoms and support timely response to changes • A comprehensive series of mindfulness resources to aid stress reduction and anxiety management • Validated assessment tools to help patients and their clinicians in the management of their condition • And much more…. Over 3,300 patients have now been registered onto myAsthma+ across the UK. A recent patient survey* found that: • 84% found the app easy to use • 72% felt they had a greater understanding about their condition since using the app • 69% felt more confident in managing their condition

Results of a service evaluation using myHeart in a large London-based acute NHS Trust. We are pleased to report the outcomes from this recent service evaluation of myHeart and the potential benefit of using the myHeart app to supplement existing cardiac rehabilitation (CR). Cardiac rehabilitation is an essential evidence-based intervention that supports patient recovery following a cardiac event. It offers patients a structured education and exercise programme to aid recovery and support behavioural changes to help reduce the risk of future cardiac health complications. The myHeart app provides a structure educational and exercise intervention that mirrors current CR service delivery as well as supportive self-management tools. Overall, 721 patients were invited to participate in 1 of 4 groups (class-based CR, class-based CR with myHeart, home-based CR and home-based CR with myHeart). A total of 584 patients opted to use class-based CR and of these 43 chose to include myHeart to support them with this. There were 137 patients in the home-based group, with 54 choosing to include myHeart alongside their CR. This 12-week evaluation involved functional, physical and psychological assessments both before and after CR to explore potential changes. Patients were also asked to complete a rating of perceived exertion Borg RPE scale (Borg 6-20). Those in the home-based groups were contacted mid-way through the study. Results identified three key outcomes: 1. Blood pressure, cholesterol, LDL, BMI, HbA1c and exercise were all very similar across the groups with marginal differences across each measure. 2. Drop-out rates (DOR) of patients being invited to attend CR and attending CR were significantly lower in those groups with access to myHeart. * Class only: DOR = 58.2% Class + App; DOR = 25.6% * Home only: DOR = 73.5% Home + App; DOR = 42.6% 3. Those patients with access to myHeart and in the home-based group saw the greatest improvement in anxiety and depression scores. This real-world evaluation provides an encouraging insight into the potential impact of myHeart to supplement CR services, and is suggestive that, as an adjunct to support both class and home-based programmes, myHeart helps to reduce drop-out rates in CR and can assist in reinforcing continuous engagement with CR programmes.