Evidence

Results of a service evaluation using myHeart in a large London-based acute NHS Trust. We are pleased to report the outcomes from this recent service evaluation of myHeart and the potential benefit of using the myHeart app to supplement existing cardiac rehabilitation (CR). Cardiac rehabilitation is an essential evidence-based intervention that supports patient recovery following a cardiac event. It offers patients a structured education and exercise programme to aid recovery and support behavioural changes to help reduce the risk of future cardiac health complications. The myHeart app provides a structure educational and exercise intervention that mirrors current CR service delivery as well as supportive self-management tools. Overall, 721 patients were invited to participate in 1 of 4 groups (class-based CR, class-based CR with myHeart, home-based CR and home-based CR with myHeart). A total of 584 patients opted to use class-based CR and of these 43 chose to include myHeart to support them with this. There were 137 patients in the home-based group, with 54 choosing to include myHeart alongside their CR. This 12-week evaluation involved functional, physical and psychological assessments both before and after CR to explore potential changes. Patients were also asked to complete a rating of perceived exertion Borg RPE scale (Borg 6-20). Those in the home-based groups were contacted mid-way through the study. Results identified three key outcomes: 1. Blood pressure, cholesterol, LDL, BMI, HbA1c and exercise were all very similar across the groups with marginal differences across each measure. 2. Drop-out rates (DOR) of patients being invited to attend CR and attending CR were significantly lower in those groups with access to myHeart. * Class only: DOR = 58.2% Class + App; DOR = 25.6% * Home only: DOR = 73.5% Home + App; DOR = 42.6% 3. Those patients with access to myHeart and in the home-based group saw the greatest improvement in anxiety and depression scores. This real-world evaluation provides an encouraging insight into the potential impact of myHeart to supplement CR services, and is suggestive that, as an adjunct to support both class and home-based programmes, myHeart helps to reduce drop-out rates in CR and can assist in reinforcing continuous engagement with CR programmes.

Results have led to continued QISMET Accreditation for myDiabetes (QIS2015) and have revealed the app could play an important role in supporting structured patient education delivery for type 2 diabetes following initial diagnosis, and as an ongoing resource. Together with a large Health and Care Partnership, we led a multi-centre service evaluation to explore the impact of myDiabetes on education course attendance rates. T2DM is a serious and growing problem worldwide and affects more than 3 million people in the UK. Structured education is a large part of managing T2DM to promote a healthy lifestyle and improve blood sugar control. However, the uptake for education courses has been less than encouraging across the UK. By offering a digital alternative or adjunct to a class-based course those who are unable or prefer not to attend a class-based programme, are able to receive structured education. myDiabetes is an app to support patients and clinicians manage diabetes together, remotely and at scale. Overall, 83 T2DM patients were recruited by the healthcare team, of which 28 chose to use myDiabetes alone, 35 chose only usual care, and 20 chose to use both. Patient education usage was monitored over a 12-week period. During this evaluation we monitored changes in diabetes related clinical health outcomes where possible, including HbA1c, blood pressure and body mass index. Participants in all three sites were asked to complete the Problem Areas In Diabetes (PAID) questionnaire at the beginning and end of the evaluation to explore markers of improvement in diabetes related distress. Results showed the app was acceptable in this care setting with 31 of 42 patients using it alone or as an adjunct to usual care. A total of 586 education videos were watched, on average each patient watched 22.5 (SD 19.6) videos. There was a reduction in PAID scores across all arms, with the app only arm showing the greatest improvement. Patients using myDiabetes showed the greatest improvement in HbA1c (-7.5 vs –4.4 mmol/mol), Systolic Blood Pressure (-12.2 vs +3.3 mmHg) and PAID score (-6.8 vs –5.2). In this real world evaluation myDiabetes performed better than published education course completion rates and resulted in significant improvements in HbA1c and PAID score compared to classed-based programs. This supports the use of myDiabetes to support the delivery of structured based education for patients with type 2 diabetes.
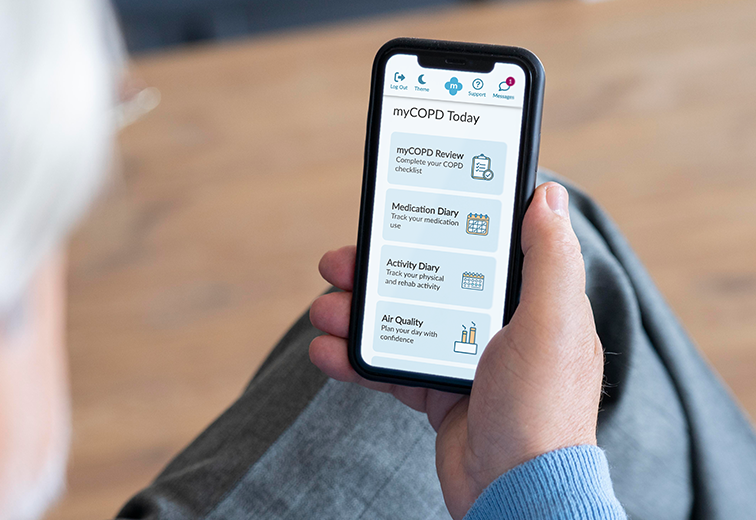
Henry M.G. Glyde1Alison M. Blythin2 Tom M.A. Wilkinson3Ian T. Nabney4 James W. Dodd5 EPSRC Centre for Doctoral Training in Digital Health and Care, University of Bristol, Bristol, UK my mHealth Limited, Bournemouth , UK my mHealth and Clinical and Experimental Science, University of Southampton, Southampton, UK School of Engineering Mathematics and Technology, University of Bristol, Bristol, UK Academic Respiratory Unit, Translational Health Sciences, Bristol Medical School, University of Bristol, Bristol, UK Abstract Background Acute exacerbations of COPD (AECOPD) are episodes of breathlessness, cough and sputum which are associated with the risk of hospitalisation, progressive lung function decline and death. They are often missed or diagnosed late . Accurate timely intervention can improve these poor outcomes. Digital tools can be used to capture symptoms and other clinical data in COPD. This study aims to apply machine learning to the largest available real-world digital dataset to identify AECOPD Prediction tool which could be used to support early intervention improve clinical outcomes. Objective To create and validate a machine learning predictive model that forecasts exacerbations of COPD 1-8 days in advance. The model is based on routine patient-entered data from myCOPD self-management app. Method Adaptations of the AdaBoost algorithm were employed as machine learning approaches. The dataset included 506 patients users between 2017-2021. 55,066 app records were available for stable COPD event labels and 1,263 records of AECOPD event labels. The data used for training the model included COPD assessment test (CAT) scores, symptom scores, smoking history, and previous exacerbation frequency. All exacerbation records used in the model were confined to the 1-8 days preceding a self-reported exacerbation event. Results TheEasyEnsemble Classifier resulted in a Sensitivity of 67.0% and a Specificity of 65% with a positive predictive value (PPV) of 5.0% and a negative predictive value (NPV) of 98.9%. An AdaBoost model with a cost-sensitive decision tree resulted in a a Sensitivity of 35.0% and a Specificity of 89.0% with a PPV of 7.08% and NPV of 98.3%. Conclusion This preliminary analysis demonstrates that machine learning approaches to real-world data from a widely deployed digital therapeutic has the potential to predict AECOPD and can be used to confidently exclude the risk of exacerbations of COPD within the next 8 days. Permission to use received from Henry Glyde. Read more on Heliyon website.
Charlotte Smith 1 Francesca D’angelo 2 University Hospital of Derby and Burton, Cardiac Rehabilitation Department, Burton Upon Trent, UK. University Hospital of Derby and Burton, Health and Wellbeing Department, Burton, UK To examine the effectiveness of physical activity outcomes using a web-based Cardiac Rehabilitation application compared with a conventional programme or a combination of both. University Hospitals of Derby and Burton NHS Foundation Trust poster presented at the BACPR Annual Conference October 5-6th 2023 Permission to use received from Charlotte Smith
Francesca D’angelo 1 Charlotte Smith 2 University Hospital of Derby and Burton, Health and Wellbeing Department, Burton, UK University Hospital of Derby and Burton, Cardiac Rehabilitation Department, Burton Upon Trent, UK. To examine the effectiveness of psychological outcomes using a web-based Cardiac Rehabilitation application compared with a conventional programme or a combination of both. University Hospitals of Derby and Burton NHS Foundation Trust poster presented at the BACPR Annual Conference October 5-6th 2023 Poster presented at the BACPR Annual Conference October 5-6th 2023 Permission to use received from Charlotte Smith

Christopher Duckworth 1 Bethany Cliffe 2. Brian Pickering 1 Ben Ainsworth 2 Alison Blythin 3 Adam Kirk 3 Adam Kirk Thomas M. A. Wilkinson 3,4,5 Michael J. Boniface 1 1 IT Innovation Centre, Digital Health and Biomedical Engineering, University of Southampton, Southampton, UK. 2. School of Psychology, Faculty of Environmental and Life Sciences, University of Southampton, Southampton, UK my mHealth Limited, London, UK. National Institute for Health Research Applied Research Collaboration Wessex, University of Southampton , Southampton , GB Faculty of Medicine, University of Southampton, Southampton , GB Mobile Health (mHealth) has the potential to be transformative in the management of chronic conditions. Machine learning can leverage self-reported data collected with apps to predict periods of increased health risk, alert users, and signpost interventions. Despite this, mHealth must balance the treatment burden of frequent self-reporting and predictive performance and safety. Here we report how user engagement with a widely used and clinically validated mHealth app, myCOPD (designed for the self-management of Chronic Obstructive Pulmonary Disease), directly impacts the performance of a machine learning model predicting an acute worsening of condition (i.e., exacerbations). We classify how users typically engage with myCOPD, finding that 60.3% of users engage frequently, however, less frequent users can show transitional engagement (18.4%), becoming more engaged immediately ( < 21 days) before exacerbating. Machine learning performed better for users who engaged the most, however, this performance decrease can be mostly offset for less frequent users who engage more near exacerbation. We conduct interviews and focus groups with myCOPD users, highlighting digital diaries and disease acuity as key factors for engagement. Users of mHealth can feel overburdened when self-reporting data necessary for predictive modelling and confidence of recognising exacerbations is a significant barrier to accurate self-reported data. We demonstrate that users of mHealth should be encouraged to engage when they notice changes to their condition (rather than clinically defined symptoms) to achieve data that is still predictive for machine learning, while reducing the likelihood of disengagement through desensitisation. Read more
Christopher Duckworth 1 Michael J Boniface 1 Adam Kirk 2 Thomas M A Wilkinson 2 3 4 IT Innovation Centre, Digital Health and Biomedical Engineering, University of Southampton, Southampton, UK. my mHealth Limited, London, UK. National Institute for Health Research Applied Research Collaboration Wessex, University of Southampton , Southampton , GB Faculty of Medicine, University of Southampton, Southampton , GB Introduction: The GOLD (Global Initiative for Chronic Obstructive Lung Disease) 2023 guidelines proposed important changes to the stratification of disease severity using the "ABCD" assessment tool. The highest risk groups "C" and "D" were combined into a single category "E" based on exacerbation history, no longer considering symptomology. Purpose: We quantify the differential disease progression of individuals initially stratified by the GOLD 2022 "ABCD" scheme to evaluate these proposed changes. Patients and methods: We utilise data collected from 1529 users of the myCOPD mobile app, a widely used and clinically validated app supporting people living with COPD in the UK. For patients in each GOLD group, we quantify symptoms using COPD Assessment Tests (CAT) and rate of exacerbation over a 12-month period post classification. Results: CAT scores for users initially classified into GOLD C and GOLD D remain significantly different after 12 months (Kolmogorov-Smirnov statistic = 0.59, P = 8.2 × 10-23). Users initially classified into GOLD C demonstrate a significantly lower exacerbation rate over the 12 months post classification than those initially in GOLD D (Kolmogorov-Smirnov statistic = 0.26; P = 3.1 × 10-2; all exacerbations). Further, those initially classified as GOLD B have higher CAT scores and exacerbation rates than GOLD C in the following 12 months. Conclusion: CAT scores remain important for stratifying disease progression both in-terms of symptomology and future exacerbation risk. Based on this evidence, the merger of GOLD C and GOLD D should be reconsidered. Read more
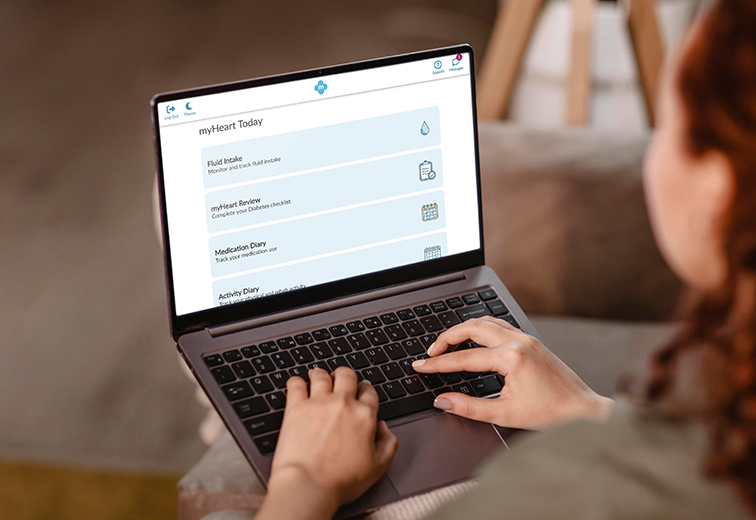
Alison M. Blythin 1 Jack Elkes 2 Ronie Walter 3 Amber Bhogal 1 Ian Thompson Thomas van Lindholm 1 Matt Smith 1 Trish Gorely 3 Tom M.A. Wilkinson 1,5 Stephen J. Leslie 3,4 and Adam Kirk 1 my mhealth Limited, London, UK Imperial College London Clinical Trials Unit, London, UK University of the Highlands and Islands, SCOTLAND NHS Highlands Cardiology Department, SCOTLAND University of Southampton Faculty of Medicine, UK COVID-19 significantly impacted cardiac rehabilitation (CR) delivery. Service disruption left numerous patients without treatment access. Many healthcare teams made use of digital apps to support CR delivery and patients remotely. This evaluation aimed to analyse digital CR access from the myHeart interactive, cloud-based self-management app during the pandemic. Five NHS secondary care CR services agreed to combine existing anonymised app data between Mar-Oct 2020 for 12-weeks to align as much as possible with traditional CR models. No statistically significant differences were observed across age groups or gender between users who activated myHeart and those who did not. N=314/350 (89.7%) users accessed 5,469 CR videos with N=313/314 (99.7%) accessing 3,606 within the first 6-weeks of activation. No statistically significant differences were observed across gender or age group for education video views. Users with angina only diagnosis accessed more exercise videos than those with other reported diagnoses. Patient user feedback responses showed a statistically significant increase in self-management confidence following myHeart access. myHeart provided remote timely CR during service disruption. This evaluation is the beginning of a journey to understand app usage however further research is needed to fully understand the role digital health can play in the delivery of CR.f your post goes he re. To edit this text, click on it and delete this default text and start typing your own or paste your own from a different source. Read more.

A.M. Blythin 1, J. Elkes 2 T. van Lindholm 1 A. Bhogal 1 T.M.A. Wilkinson 1 C. Saville 3 A. Kirk 1 Department of Research & Innovation, my mhealth Limited, Bournemouth, UK. School of Public Health, Imperial College Clinical Trials Unit, London, UK. Faculty of Medicine, University of Southampton, Southampton, Hampshire, UK Digital health interventions provide a potential solution to improve diabetes education delivery at population scale, overcoming barriers identified with traditional approaches. This evaluation analysed usage data for people with type 2 diabetes focusing on digital structured diabetes education. Results showed a positive uptake and usage with myDiabetes, with increases in app activity post-COVID. No statistically significant differences were observed between gender or age for those activated. No statistically significant differences observed in education video views across age groups, gender, diabetes treatment type or smoking status. The findings support the use of digital health in the provision of additional support for the delivery of diabetes education. There is potential for increasing diabetes education rates by offering patients a digital option in combination with traditional service delivery which should be substantiated through future research. Read more
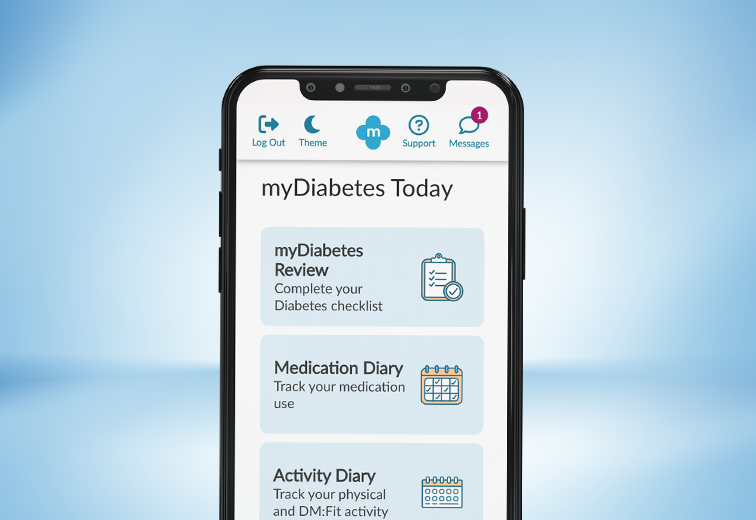
Published in Nature on 7 March 2022 A. Geirhos 1 M. Stephan 2 M. Wehrle 3 et al Sci Rep 12, 3639 (2022). Department of Clinical Psychology and Psychotherapy, Institute of Psychology and Education, Faculty of Engineering, Computer Science and Psychology, Ulm University, Ulm, Germany Department of Rehabilitation Psychology and Psychotherapy, Albert-Ludwigs University Freiburg, Freiburg, Germany Department of Clinical Psychology and Psychotherapy, Institute of Psychology and Education, Faculty of Engineering, Computer Science and Psychology, Ulm University, Ulm, Germany Mobile health applications (MHA) have been found to be a promising technological approach to support self-management. A German study has revealed results from an evaluation of diabetes self-management mobile health applications. The Mobile App Rating Scale (MARS), rated on a 5-point scale, was used for analysis. 120 mobile health apps from the European Google Play Store and the Apple App store were included. Results identified myDiabetes as highest of all 120 evaluated mobile health apps, according to: Quality Concordance with recommended self-management tasks Implementation of persuasive system design principle myDiabetes overall MARS Score = 4.62 Permission to use received from Dr L. B. Sander Read more on Nature
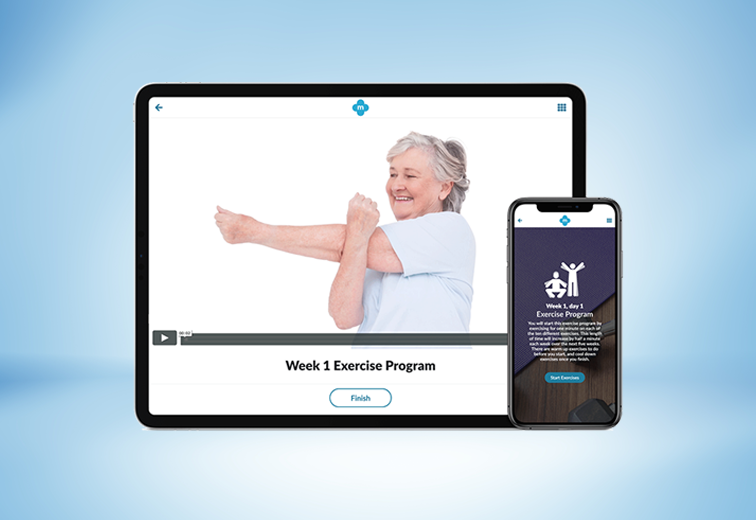
Results of a service evaluation by Southend University Hospital using myCOPD to support a home-based pulmonary rehabilitation (PR) programme in several different local locations. The Enhanced Pulmonary Rehabilitation Programme was launched by Southend University Hospital in 2018. The programme was designed to offer a variety of options for patients to complete their PR. This was a new model of care offered to patients who were unable to attend or were waiting for a centre-based course. This provided these patients with an opportunity to undertake an education and exercise course at home, supported by the PR team. The home-based PR programme recruited 88 patients to the evaluation. 59 of the 88 home-based PR patients chose to include myCOPD , of which 15 (17%) used myCOPD only and 44 (50%) used it in combination with written information and a DVD. The remaining 29 home-based patients did not wish to include myCOPD in their PR programme and were therefore provided with either written information or a DVD. Home-based completion rates showed that 31 (52.5 %) of the 59 patients using myCOPD at home completed the full PR programme in comparison to 7 (24.1%) of 29 who did not include the app. The COPD Assessment Test (CAT) was used as an outcome measure to explore the impact of the app for those at home. Results showed that all home-based groups saw an improvement in CAT score, however the greatest improvement overall was in the myCOPD alone group with a -3.7 point reduction. CAT score reduction across other groups ranged from -3.6 to -1.9. Despite small differences observed in CAT score between groups, there was a more than a 100% higher completion rate of the full PR programme in those using myCOPD compared to those who did not. The app has a structured PR programme for patients to follow at a time that suits them demonstrating the apps diverse capability. In-app notifications can be sent to remind patients to complete their PR programme and clinicians can monitor their progress. This evaluation supports the significant impact that the myCOPD app can provide to support patients and healthcare service delivery remotely and at scale across different locations. The evaluation also supports the findings from the much larger Trooper Study published in bmj.com.

Simon Bourne 1,2 Ruth DeVos 1,2 Malcolm North 2 Anoop Chauhan 1 Ben Green 1 Thomas Brown 1 Victoria Cornelius 3 Tom Wilkinson 2,4 Portsmouth Hospitals NHS Trust, Portsmouth, UK my mhealth Ltd Bournemouth, UK Imperial College, London, UK Clinical and Experimental Sciences, Faculty of Medicine, University of Southampton, Southampton, UK
Mal North 1 Simon Bourne 1 Ben Green 2 Anoop J. Chauhan 2 Tom Brown 2 Jonathan Winter 2 Tom Jones 2 Dan Neville 2 Alison Blythin 1 4, 5 Matthew Johnson 4 David Culliford 4 Jack Elkes 3 Victoria Cornelius 3 Tom M. A. Wilkinson 1, 2, 5 my mhealth Ltd Bournemouth, UK Portsmouth Hospitals NHS Trust, Portsmouth, UK Imperial College, London, UK NIHR ARC Wessex, University of Southampton, Southampton, UK Faculty of Medicine, University of Southampton, Southampton, UK First publication of complete results shows the myCOPD app could play an important role in supporting recovery following an exacerbation of COPD. The results from the RESCUE trial (MMH-R02), investigating the possible impact of myCOPD in supporting the recovery of patients admitted with an exacerbation of COPD were published in NPJ Digital Medicine Journal. Exacerbations of COPD are one of the commonest causes of admission and re-admission to hospital. The role of digital interventions to support self-management in improving outcomes is uncertain. We conducted an open, randomised controlled trial of myCOPD in 41 COPD patients recruited following hospital admission with an acute exacerbation. Subjects were randomised to either receive usual care, including a written self-management plan (n=21), or the myCOPD app (n=20) for 90 days. The primary efficacy outcome was recovery rate of symptoms measured by COPD Assessment Test (CAT) score. Exacerbations, readmission, inhaler technique quality of life and patient activation (PAM) scores were also captured. Results showed the app was acceptable in this care setting and was used by 17 of the 21 patients with sustained use over the study period. The treatment effect on CAT score was 4.49 (95% CI: -8.41, -0.58) points lower in the myCOPD arm. Patients’ inhaler technique improved in the digital intervention arm (101 improving to 20 critical errors) compared to usual care (100 to 72 errors). Exacerbations tended to be less frequent in the digital arm compared to usual care; 34 vs 18 events. Hospital re-admissions risk was 30 numerically lower in the digital intervention arm: OR for readmission 0.383 (95%CI 0.074, 1.987; 31 n=35). In this feasibility study of the digital self-management platform myCOPD, the app has proven acceptable. Its use has improved exacerbation recovery rates, with strong signals of lower re-exacerbation and re-admission rates over 90 days. myCOPD reduced the number of critical errors in inhaler technique compared to usual care with written self-management. This provides a strong basis for further exploration of the use of app interventions in the context of recently hospitalised patients with COPD.

Michael Crooks 1 Jack Elkes 2 William Storrar 3 Kay Roy 4 Mal North 5 Alison Blythin 5 Alastair Watson 6 Victoria Cornelius 2 Tom M.A. Wilkinson 5, 6 Hull York Medical School, Hull, UK Imperial College London, London, UK Hampshire Hospitals NHS Foundation Trust – Basingstoke Hospital, Basingstoke, UK West Hertfordshire Hospital NHS Trust – Hemel Hempstead Hospital, Hemel Hempstead, UK mymhealth Limited, Bournemouth, UK University of Southampton Faculty of Medicine, Southampton, UK First publication of complete results for a preliminary trial of a self-management intervention using a scalable app ( myCOPD) demonstrated signals of potential clinical benefit in a population of patients with mild-moderate and newly diagnosed COPD over a 90 day period. The results from the EARLY trial (MMH-R03), funded by an UKRI Innovate UK Grant to my mhealth were published in ersjournals.com. Self-management interventions in COPD aim to improve patients’ knowledge, skills and confidence to make correct decisions, leading to an improvement in health status and outcomes. myCOPD is a web-based self-management app known to improve inhaler use and exercise capacity in individuals with more severe COPD. We explored its impact in patients with mild-moderate or recently diagnosed COPD through a 12-week, open-label, parallel-group, randomised-controlled trial of myCOPD compared with usual care. The co-primary outcomes were between group differences in mean COPD assessment test (CAT) score at 90 days and critical inhaler errors. Key secondary outcomes were app usage and patient activation measurement (PAM) score. 60 patients were randomized overall (29 myCOPD, 31 usual care). Groups were balanced for FEV1% predicted, but baseline imbalance between groups for exacerbation frequency and CAT score. There was a trend to lower CAT scores in the myCOPD arm, but due to the size of the study there was no significant adjusted mean difference in CAT score at study completion, -1.27 (95% CI -4.47 to 1.92, p=0.44) lower in myCOPD. However, increasing app use was associated with greater CAT score improvement. The odds of ≥1 critical inhaler error was much lower in the myCOPD arm (adjusted odds ratio of 0.30 (0.09; 1.06, p=0.061)). The adjusted odds ratio for being in a higher PAM level at 90 days was 1.65 (0.46; 5.85) in favour of myCOPD. The small sample size and phenotypic difference between groups limited our ability to demonstrate statistically significant evidence of benefit beyond inhaler technique, this confirms the finding from previous studies that myCOPD can reduce inhaler technique errors by >70%. The findings of this study will now be used to power a much larger RCT to investigate the impact of myCOPD in this patient population.

O’Sullivan C 1 Stokes J 2 Blythin A 2 Dr. Kirk A 2 Dr. Ellison P 3 Marine and Oakridge Surgeries, South Coast Medical Group, Dorset my mhealth Limited, Bournemouth Dorset Intelligence & Insight Service, Our Dorset – Digital ‘Our Digital Dorset’ and ‘my mhealth’ conducted a study exploring the usage of myCOPD by tracking activity using the Dorset Intelligence and Insight Service (DiiS). Results showed positive uptake and usage with myCOPD, demonstrating improvement in CAT scores. Socioeconomic factors did not appear to negatively influence app activation. myCOPD supports the remote monitoring of patients with COPD. App activity and changes in CAT score were visible to clinicians through DiiS, contributing to a positive population health management approach.

Francis P Chmiel 1 MSc, DPhil; Dan K Burns 1 MSc, PhD; John Brian Pickering 1 DPhil; Alison Blythin 2 MRES; Thomas MA Wilkinson 2,3,4* PhD; Michael J Boniface 1* BEng School of Electronics and Computer Science, University of Southampton , Southampton , GB my mHealth Limited, Bournemouth , GB National Institute for Health Research Applied Research Collaboration Wessex, University of Southampton , Southampton , GB National Institute for Health Research Applied Research Collaboration Wessex, University of Southampton , Southampton , GB
R esearch MMH-R06 published in Published on Pub Med 24th October 2023 Christopher Duckworth 1 Michael J Boniface 1 Adam Kirk 2 Thomas M A Wilkinson 2 3 4 IT Innovation Centre, Digital Health and Biomedical Engineering, University of Southampton, Southampton, UK. my mHealth Limited, London, UK. National Institute for Health Research Applied Research Collaboration Wessex, University of Southampton , Southampton , GB Faculty of Medicine, University of Southampton, Southampton , GB
Results of a supported self-management evaluation of COPD patients by Stonehaven Medical Group and Aberdeenshire Health & Social Care Partnership (NHS Grampian). Kris McLaughlin, Erika Skinner Stonehaven Medical Group and Aberdeenshire Health & Social Care Partnership designed this test of change evaluation to explore the impact of myCOPD on patient self-management, exacerbations frequency, unscheduled general practice (GP) consultations and hospital admissions. Chronic Obstructive Pulmonary Disease (COPD) is a common and serious disease of the lungs. Many people in the UK suffer with the disease and it is a leading cause of hospital admissions. Preventing COPD exacerbations and promoting overall wellbeing can be achieved through supportive self-management of disease. However, successful self-management is dependent on the knowledge and skills provided to patients to give them the confidence to make the right decisions about their treatments, use of healthcare services and lifestyle choices. Digital tools can be a useful resource to support patient self-management. The myCOPD app provides structured education, pulmonary rehabilitation, inhaler videos to promote good inhaler technique as well as supportive self-management tools. This test of change evaluation was conducted in primary care in 2019. At 5 months data was collected to review any outcomes since myCOPD was introduced. Overall, 64 patients agreed to take part with 43 agreeing to an early review. Of these 43, 23 (53.4%) patients who had been given access to myCOPD attended the interim review. The evaluation involved measuring CAT score, inhaler technique including rescue inhaler usage, healthcare usage and hospital admissions, and patient feedback. Results identified 4 key outcomes: 1. An overall improvement in mean CAT score of -2.1 since the start of the study 2. A mean reduction in rescue inhaler use was observed from 3.17 to 2.13, demonstrating an improvement in symptom control. There was also an overall improvement in inhaler technique, where good inhaler technique practices increased from 48 to 91% 3. There was a reduction observed in healthcare usage when comparing patient data prior to myCOPD. Overall, there were 20 (19%) less unscheduled GP appointments (reduction range of 105 to 85), and hospital admissions dropped from 6 to 0 during this time 4. Patient feedback showed that the proportion of patients who described their ability to manage exacerbations very well rose from 29 to 55%, and those who felt confident using an inhaler rose from 76 to 90% This real-world evaluation of myCOPD provides valuable insights into the benefits of using digital health to support self-management. Recent studies have shown that myCOPD can provide patients with an alternative, or adjunct, to their COPD healthcare management. These results reinforce the evidence base from our formal RCTs (EARLY and RESCUE) which showed that using myCOPD improved inhaler technique, reduced CAT score, exacerbations and hospital admissions. Based on these results, Stonehaven Medical Group, NHS Grampian’s Respiratory Managed Clinical Network canvassed for widespread adoption of myCOPD. This is to be commissioned by the Operation Home First Steering Group who have approved funding to enable rapid deployment of myCOPD during winter 2020/21.