The NHS is facing unprecedented pressures this winter, and it is anticipated that patients with respiratory disease may occupy up to half of all hospital beds. It is therefore vital that the management of patients with Severe Asthma, who are at high risk of hospitalisation, is optimised.
In this context, the Accelerated Access Collaborative (AAC), Academic Health Sciences Network (AHSN), my mhealth Limited and University Hospitals Southampton (UHS) are pleased to announce the launch of myAsthma Biologic, an extension to my mhealth’s existing myAsthma product, which will support 10,000 patients with severe asthma on biologic therapy across the United Kingdom.
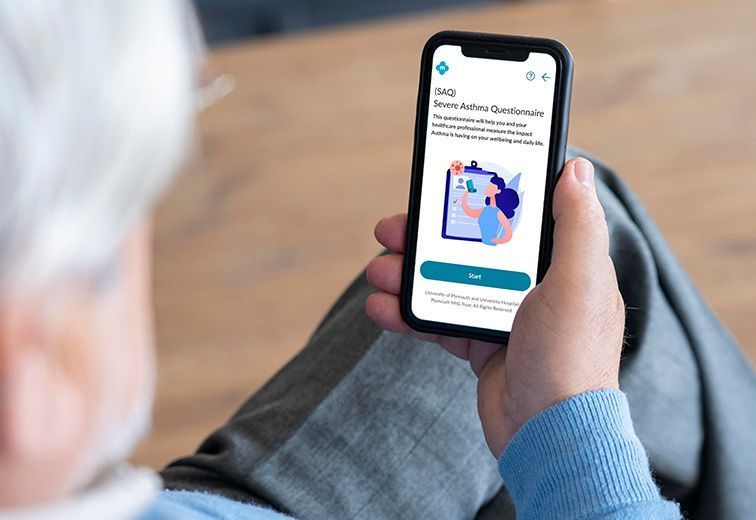
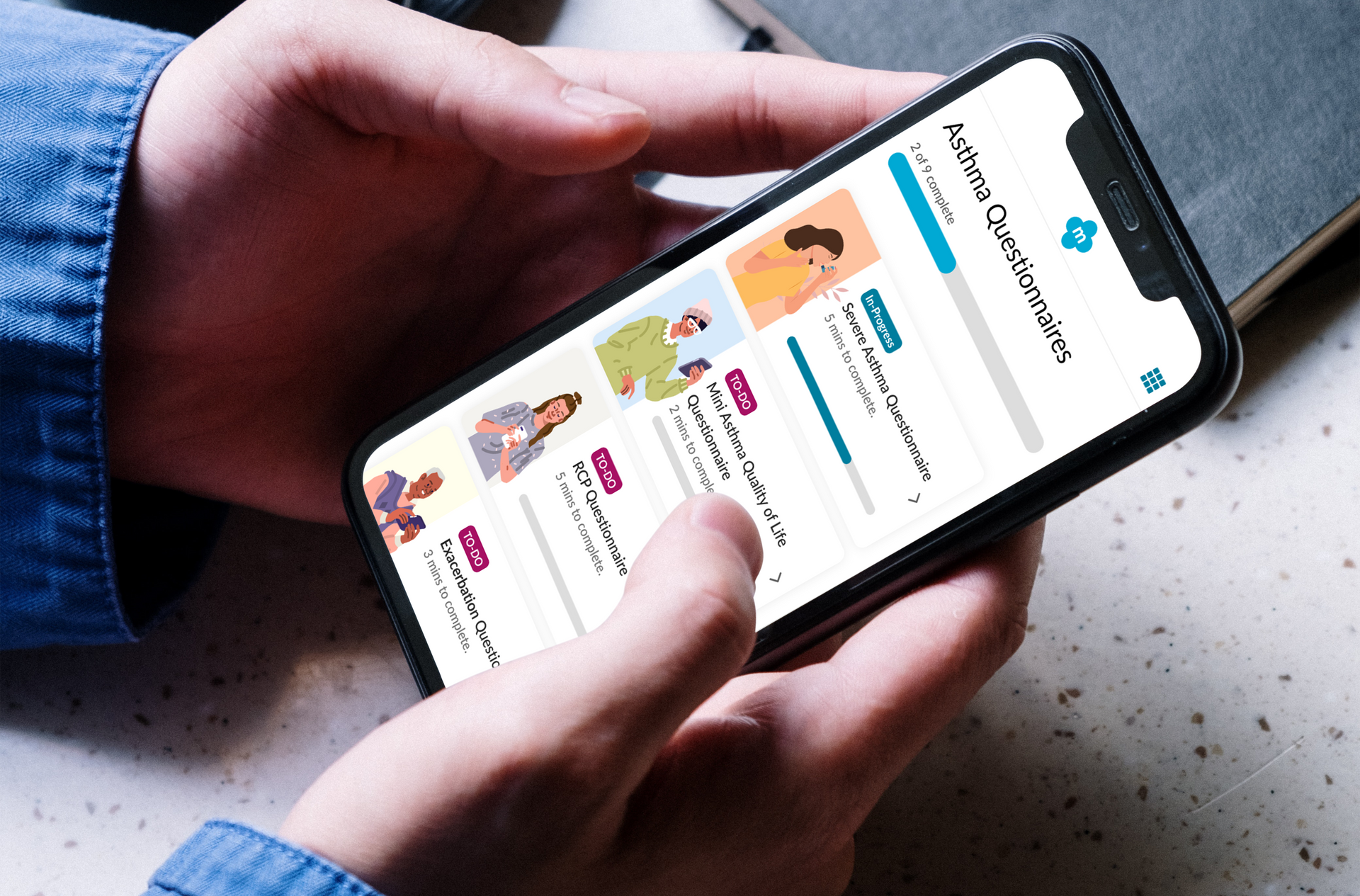
Over the last few years, the administration of biologic therapy has moved from the clinic, into the home. This is far more convenient for patients, who in many cases had to travel hundreds of miles to receive their treatment because it is only offered in a few specialist centres. myAsthma Biologic was commissioned as part of the NHS AAC Rapid Uptake Products programme, which aims to improve access to biologic therapies by improving pathways and current practices to achieve timely specialist patient care. The digital therapeutic supports patients in managing their asthma, and their clinical teams in managing and monitoring them remotely.
This exciting new product will also facilitate standardised and timely collection of clinical data through automated upload to the national severe asthma registry. Through the programme, sites currently inputting data in the severe asthma registry and prescribing asthma biologics will have access to myAsthma Biologic.