What is the role of a Digital Health Adviser?
How to make digital transformation work and increase engagement with digital technology
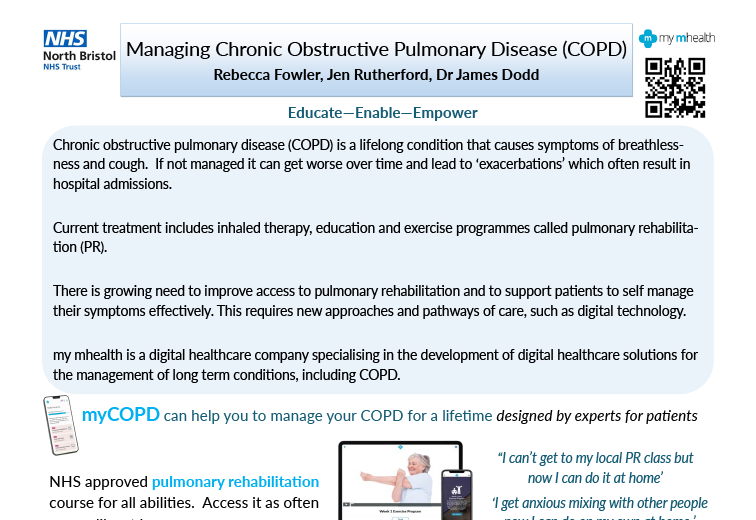
my mhealth is a clinically led software company that develops and deploys apps which help patients and clinicians to manage long-term conditions better. Since our launch we have worked collaboratively with 100s of CCGs, NHS Acute Trusts, GP practices and community providers to digitally transform the way they provide care and interact with individuals with long-term conditions.
Through this process we have developed a great insight into how to make digital transformation work and remove some of the barriers which can prevent uptake of and engagement with digital technology.
One of the most impactful interventions is the development of a new Digital Health Adviser (DHA) role.
A DHA is typically a non-clinical member of staff who is trained by the my mhealth digital transformation team to work with both clinicians and patients to improve uptake and engagement with our apps.

- Supporting the process of patient identification and enrolment
- Following up patients, troubleshooting any problems they may have and signposting them to the most relevant parts of the self-management platform
- Supporting clinicians to optimally use the platform - helping them to remotely monitor and manage their patients
- 100% increase in the rate of uptake of our Apps
- 95% conversion of patient registrations into regular active users
- Activation has gone from 127 to 140, a 10.2% increase within 48 hours of re-activation sent.
- 38 patients have logged on to the app within 48 hours of contact.
- The number of educational videos watched in 48 hours has doubled!
- For me this has been amazing. I have always been passionate about working with patients to manage their long-term conditions and this has shown me that if I do this with every provider, I can help patients to use digital technologies at massive scale."