my mhealth partner with Breezometer to provide hyper-local air quality forecasts for patients with COPD, Asthma, Diabetes and Heart Disease
Hyper-local air quality forecasts are important to patients with long-term conditions, Dr Simon Bourne explains why.
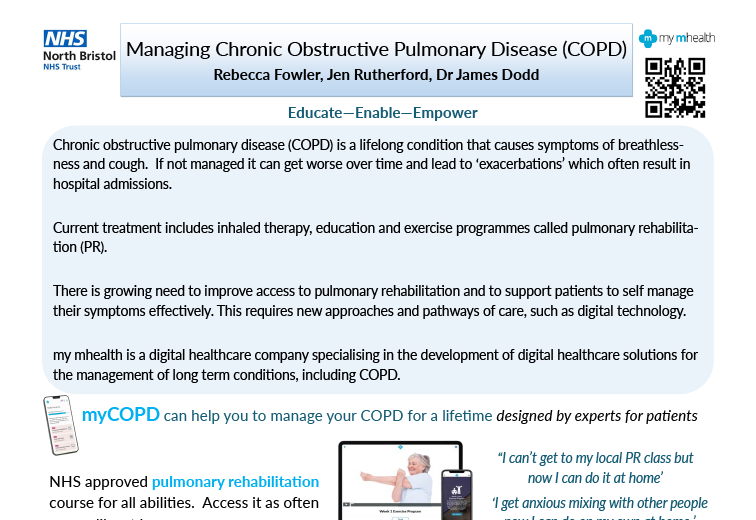
In March 2020, my mhealth released a ground-breaking hyper-local air quality forecast feature in their apps for patients. Partnering with BreezoMeter, the only company in the world who's forecasts are externally validated for accuracy and are recognised as the industry standard for real-time, location-based, outdoor air quality data, the new release is available to all existing and new users.
Leveraging BreezoMeter's Global Air Quality Index (AQI), my mhealth offer patients detailed air quality forecasts, so they know what’s in their air, exactly where they are, and understand how it affects their condition.
myCOPD and myAsthma now provide air quality information at the level of a few steps away
With actionable, personal recommendations based on individual sensitivities, and at a resolution of 5 metres - the equivalent of just a few steps - Asthma and COPD patients will be able to make informed decisions about their day-to-day activity and will be better prepared to manage their condition.
But what is the impact of poor air quality? All of us know that air pollution is bad for us, but few of us understand the true scale of impact.
Official statistics from the World Health Organisation state that 92% of us live in areas where air pollution exceeds the guidelines considered to be safe, 9/10 people breathe polluted air each day, and that 4.2 million premature deaths occur each year as a result of exposure to air pollution.
Prolonged and even short-term exposure can particularly harm sensitive groups with pre-existing respiratory or cardiovascular conditions, the elderly, children, and pregnant women, however, the stark reality is air pollution exposure affects our bodies from head to toe - research has found air pollution to be linked to cancer, asthma, strokes, dementia and more.
Ran Korber, CEO of Breezometer told us:
"Today, all of our environmental engineers understand the connection between our health and the environment and refuse to compromise when it comes to accuracy around air quality & helping people to manage exposure. After all, we each breathe 3000 gallons of air a day."
BreezoMeter adopts an innovative approach to air quality data reporting. They combine data from multiple data sources, which includes more than 47,000 sensors worldwide, meteorological data, satellites, weather, fire and sandstorm events, and live traffic information. This unique approach means they're able to collect information even when one source becomes unavailable.
They calculate air pollution in 440 million geographical points around the world and validate and organize more than 1.8 TB of data each hour. They deploy 35 different algorithms, machine-learning and sophisticated modelling to calculate 7.5 billion pollutant concentrations in high accuracy on an hourly basis. The end result is real-time air quality information that is accurate down to a hyper-local scale of 0.3 Miles (500 Meters).

Dr Simon Bourne, CEO and founder of my mhealth goes into more detail about the importance of hyper-local air quality forecasts for patients, "There has been a rapidly evolving evidence base that links poor air quality to worse outcomes for a patient with long-term conditions. We have partnered with BreezoMeter to provide our patients with access to the very best in local air quality information, right down to the type of pollution so our patients can make an informed choice about how they plan their day. There is currently no other long-term condition platform that delivers this information, with this accuracy and in such detail".
Dr Bourne has big plans for the new air quality feature in the apps, with detailed pollution forecasts helping thousands of more patients when my mhealth expand overseas into territories such as The USA, Australia and New Zealand.
"Another reason why this implementation is so important is that we have near-term plan plans to expand our business overseas this year. This partnership will enable us to deliver the same accuracy of forecasting wherever you are in the world"
If you're a healthcare professional or clinician and want to know more about how hyper-local air pollution forecasting can help your asthma and COPD patients, or if you're living with one of these conditions and would like to benefit from the new feature in the myCOPD and myAsthma apps, you can find out more at www.mymhealth.com or by calling my mhealth on 0044 (0)1202 299 583