Last week,
Waterside PCN became the first PCN in the UK to go live with the
my mhealth COVID-19 Virtual Ward app. Waterside PCN is a group of 5 surgeries based in West Hampshire, who have started digitally transforming their patient pathway, by providing their patients with access to our entire Long-Term Condition (LTC) platform. Patients suspected to have, or diagnosed with coronavirus, will now have access to the COVID-19 Virtual Ward alongside the other apps.
The COVID-19 Virtual Ward app uses a clinically recognised scoring algorithm to assist patients being managed in a virtual environment to be cared for remotely by their clinical team. By answering questions and recording a few measurements twice a day using a pulse oximeter, the patients provide their clinical team with the information needed to monitor their symptoms remotely.
"The app has enabled us to monitor patients safely at home who we otherwise would have either needed to bring back daily for saturation monitoring or would have required admission."
The Waterside PCN team provided patients with access to a pulse oximeter, enabling them to accurately measure their oxygen levels and add their results to the Covid-19 virtual ward.
We asked Dr Jessica Pickford, of the Red and Green Practice, to tell us how the app is helping her patients. She told us:
"The Waterside PCN has been itching to get going with the LTC apps since we discovered them towards the tail end of last year. The final trigger was the onset of the COVID-19 pandemic and the subsequent development of the COVID-19 Virtual Ward app. The combination of these apps provided an instant set of solutions to an acute and unprecedented set of complex problems not seen on this scale in primary care before."
With the nation in lockdown, how were we going to provide the same level of care and monitoring to our patients with LTCs? The very people who are deemed most vulnerable and in most need of regular health provision now find themselves in the position of being put at risk by just coming to the surgery. Of course, the other, more acutely worrying dilemma was how were we to effectively monitor those patients in the community with potential COVID-19 infection?
We know from the evidence coming out of China and Italy that people with COVID-19 can show quite mild symptoms one day and then be very unwell requiring hospitalisation within 48hours. One of the earliest signs of deterioration is a drop in their oxygen saturations which is often not associated, at least initially, with a worsening of symptoms. How were we going to keep patients at home that could be following this path? The solution came with the COVID-19 Virtual Ward app. Following remote telephone triage, the practices within the network can issue patients with potential COVID-19 symptoms pulse oximeter and a thermometer. These are then collected from the hot site by a family member or friend. This enables the patient to input their observations into the COVID-19 app and score their symptoms. Algorithms within the app then presents relevant alerts and advice to the patient and present this within a dashboard that can be visualised remotely from the hot hub.
"The app has enabled us to monitor patients safely at home who we otherwise would have either needed to bring back to the hot hub daily for saturation monitoring or would have required admission. It also allows us to react quickly to those patients who are showing the early signs of deterioration but who would otherwise not seek help."
We have been able to utilise the long-term apps alongside the COVID-19 Virtual Ward app in several ways. Firstly, that people with diabetes are at increased risk of hyperglycaemia and Diabetes Ketoacidosis (DKA) with COVID-19. Combining the myDiabetes app with the COVID-19 Virtual Ward app assists the GP in monitoring people with diabetes who develop COVID-19 closely and again enables them to react quickly and admit the patient if needed.
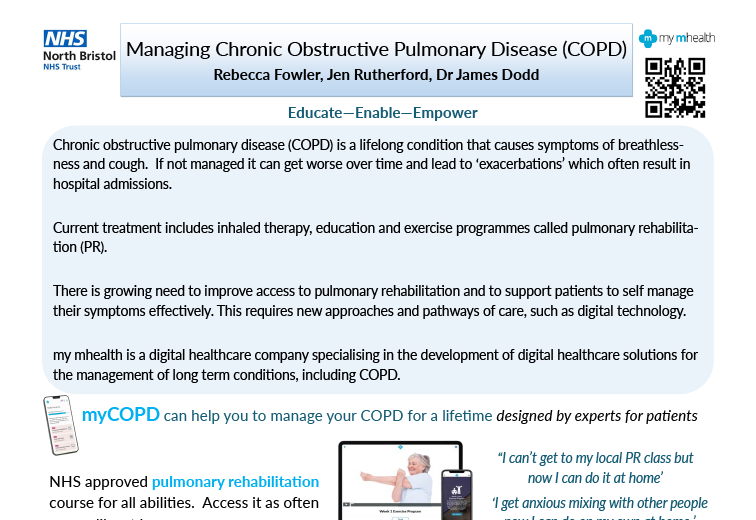
Secondly, with regards to patients with Chronic Obstructive Pulmonary Disease (COPD) and asthma, it can be difficult to determine if their symptoms are just due to an exacerbation of their LTC or if it is the early signs of COVID-19. By combining the two apps we can safely monitor observations and symptoms for the potential of COVID-19 whilst assisting with the management of their LTC.
We have been very clear to patients that they are to not rely on the clinician monitoring the dashboard but should note the prompts generated by the apps and react accordingly. We promote the persons ’ownership’ of their LTC and the apps are a perfect platform for this. They are full of self-help videos, education and self-management opportunities. The dashboard gives the clinician a very quick and simple overview of the patient data within the individual apps enabling quick decisions and support.
Aside from COVID-19, the LTC apps provide us with a solution to the issue of maintaining LTC support and advice whilst working in a remote environment. Our patients have found the apps very simple to set up. Patients of all ages are utilising them with ease and are excited to use them. Our diabetes, asthma and COPD nurses can also benefit from having our patients use these apps. Not only do the apps assist with the accumulation of data remotely, but they also improve the patient's engagement, insight and management of their own health, and save us significant amounts of time trying to collate all the relevant information for the yearly reviews and QOF. The apps are revolutionising our way of working and improving our patient care."